Summary Statement
This physician presentation is about the risks of developing addiction from over-prescribing opioid pain medication for work-related injuries and for chronic pain addresses employers. In addition to identifying high quality Employee Assistance Programs, the power-point presentation provides current CDC guidance, recommendations for supervisor training, and an extensive reference list. There are no accompanying notes, and acronyms may not be immediately recognized.
January 25, 2017
Don Teater MD
Teater Health Solutions
Disclosure:I have nothing to disclose. All states have different laws regarding drug free workplace procedures and drug testing. You should always consult an attorney with expertise in DFWP when developing a workplace policy.
Opioid increase
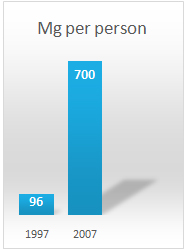
Drug distribution through the pharmaceutical supply chain was the equivalent of 96 mg of morphine per person in 1997 and approximately 700 mg per person in 2007, an increase of >600%.2
Our rate of opioid prescribing his increased from an average of 96 morphine mg equivalents per person in 1997 to over 700 mg per person in 2007. That is an increase of greater than 600%2. That is enough opioids for every man, woman, and child in United States to take Vicodin around-the-clock for over one month.
Opioid facts
The United States has 4.6% of the world’s population.
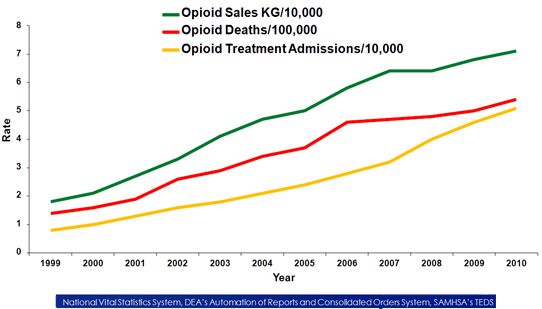
Rates of opioid overdose deaths, sales and treatment admissions, US, 1999-2010.7
The State of US Health5
Years lived with disability (in thousands)
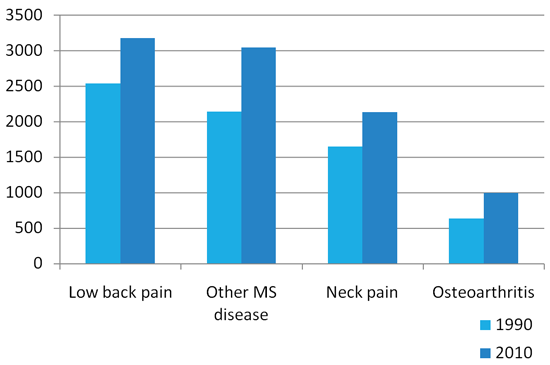
US Burden of Disease Collaborators. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA. 2013 Aug 14;310(6):591-608. doi: 10.1001/jama.2013.13805. PubMed PMID: 23842577
Prevalence
-
About 1% of the U.S. adult population is addicted to these medications.
-
About 2% of working age adults.
Opioids from the poppy plant for use for pain
Pain: An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage. International Association for the Treatment of Pain.
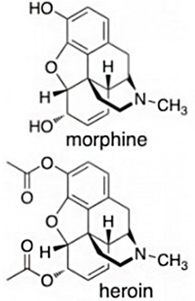 Common Opioids
Common Opioids
- Morphine
- Oxycodone
- OxyContin
- Percocet
- Hydrocodone
- Vicodin
- Zohydro
- Dilaudid (hydromorphone)
- Opana (oxymorphone)
- Fentanyl
- Methadone
Societal costs (annual)
$55.7 billion (2007):
- $25.6 billion (46%) was attributable to workplace costs.
- May be up to $11,000 per year for each drug using employee
- 24 cents per MME.
- $54 for a bottle of 30 Percocet (5mg)
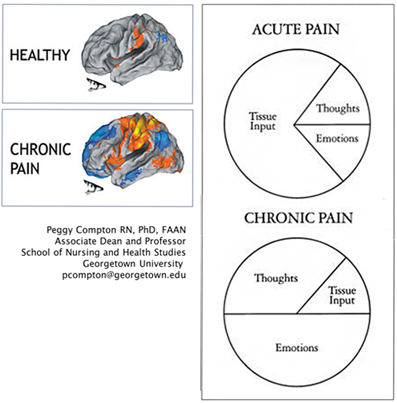
Pain
- Acute pain: Pain < 3 months
- Chronic pain: Pain > 3 months
Chronic pain "feels" different
Acute prescriptions
- Approximately 30% of ALL ER visits end with a prescription for a opioid.1
- Approximately 60% of patients going to the ER with back pain will get an opioid prescription.2
- Primary care doctors give opioids to about 35% of their patients presenting with back pain.
- Pain is the most common reason for people to go to the ER or to their primary care doctor.
The problem with opioids for acute pain
- Mentally impairing
- Delay recovery
- Increase medical costs
- Increase the risk of future surgery
- Opioid hyperalgesia
- Double the chance of disability
- Increase falls
- They treat depression and anxiety
- Addiction
- Neurobiologic changes
- Increase all-cause mortality
One opioid prescription after an injury:
- Increases medical costs by 30%15
- Increases the risk of surgery by 22%15
- Doubles the risk of being disabled at one year42
Kaplan-Meier curve for early reimbursement for opioid prescription
Claim closure by opioid prescription
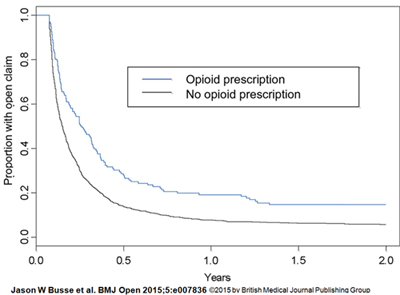
Abstract
Objective: To assess the association between early reimbursement for physiotherapy, chiropractic and opioid prescriptions for acute low back pain (LBP) with disability claim duration.
Design: Observational cohort study.
Setting and participants: From a random sample of 6665 claims for acute, uncomplicated LBP approved by the Ontario Workplace Safety and Insurance Board (WSIB) in 2005, we analysed 1442 who remained on full benefits at 4 weeks after claim approval.
Primary outcome measure: Our primary outcome was WSIB claim duration.
Results: We had complete data for all but 3 variables, which had <15% missing data, and we included missing data as a category for these factors. Our time-to-event analysis was adjusted for demographic, workplace and treatment factors, but not injury severity, although we attempted to include a sample with very similar, less-severe injuries. Regarding significant factors and treatment variables in our adjusted analysis, older age (eg, HR for age ≥55 vs <25=0.52; 99% CI 0.36 to 0.74) and WSIB reimbursement for opioid prescription in the first 4 weeks of a claim (HR=0.68; 99% CI 0.53 to 0.88) were associated with longer claim duration. Higher pre-disability income was associated with longer claim duration, but only among persistent claims (eg, HR for active claims at 1 year with a pre-disability income >$920 vs ≤$480/week=0.34; 99% CI 0.17 to 0.68). Missing data for union membership (HR=1.27; 99% CI 1.01 to 1.59), and working for an employer with a return-to-work programme were associated with fewer days on claim (HR=1.78; 99% CI 1.45 to 2.18). Neither reimbursement for physiotherapy (HR=1.01; 99% CI 0.86 to 1.19) nor chiropractic care (HR for active claims at 60 days=1.15; 99% CI 0.94 to 1.41) within the first 4 weeks was associated with claim duration. Our meta-analysis of 3 studies (n=51 069 workers) confirmed a strong association between early opioid use and prolonged claim duration (HR=0.57, 95% CI 0.48 to 0.69; low certainty evidence).
Conclusions: Our analysis found that early WSIB reimbursement for physiotherapy or chiropractic care, in claimants fully off work for more than 4 weeks, was not associated with claim duration, and that early reimbursement for opioids predicted prolonged claim duration. Well-designed randomised controlled trials are needed to verify our findings and establish causality between these variables and claim duration.
http://dx.doi.org.libproxy.lib.unc.edu/10.1136/bmjopen-2015-007836 Busse JW, Ebrahim S, Heels-Ansdell D, Wang L, Couban R, Walter SD. Association of worker characteristics and early reimbursement for physical therapy, chiropractic and opioid prescriptions with workers’ compensation claim duration, for cases of acute low back pain: an observational cohort study. BMJ Open. 2015;5(8):e007836. doi:10.1136/bmjopen-2015-007836.
The association between early opioid use/prescription and claim duration
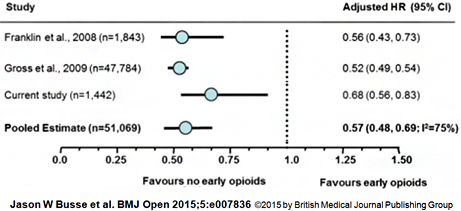
Abstract
Objective: To assess the association between early reimbursement for physiotherapy, chiropractic and opioid prescriptions for acute low back pain (LBP) with disability claim duration.
Design: Observational cohort study. Setting and participants From a random sample of 6665 claims for acute, uncomplicated LBP approved by the Ontario Workplace Safety and Insurance Board (WSIB) in 2005, we analysed 1442 who remained on full benefits at 4 weeks after claim approval.
Primary outcome measure: Our primary outcome was WSIB claim duration.
Results: We had complete data for all but 3 variables, which had <15% missing data, and we included missing data as a category for these factors. Our time-to-event analysis was adjusted for demographic, workplace and treatment factors, but not injury severity, although we attempted to include a sample with very similar, less-severe injuries. Regarding significant factors and treatment variables in our adjusted analysis, older age (eg, HR for age ≥55 vs <25=0.52; 99% CI 0.36 to 0.74) and WSIB reimbursement for opioid prescription in the first 4 weeks of a claim (HR=0.68; 99% CI 0.53 to 0.88) were associated with longer claim duration. Higher pre-disability income was associated with longer claim duration, but only among persistent claims (eg, HR for active claims at 1 year with a pre-disability income >$920 vs ≤$480/week=0.34; 99% CI 0.17 to 0.68). Missing data for union membership (HR=1.27; 99% CI 1.01 to 1.59), and working for an employer with a return-to-work programme were associated with fewer days on claim (HR=1.78; 99% CI 1.45 to 2.18). Neither reimbursement for physiotherapy (HR=1.01; 99% CI 0.86 to 1.19) nor chiropractic care (HR for active claims at 60 days=1.15; 99% CI 0.94 to 1.41) within the first 4 weeks was associated with claim duration. Our meta-analysis of 3 studies (n=51 069 workers) confirmed a strong association between early opioid use and prolonged claim duration (HR=0.57, 95% CI 0.48 to 0.69; low certainty evidence).
Conclusions: Our analysis found that early WSIB reimbursement for physiotherapy or chiropractic care, in claimants fully off work for more than 4 weeks, was not associated with claim duration, and that early reimbursement for opioids predicted prolonged claim duration. Well-designed randomised controlled trials are needed to verify our findings and establish causality between these variables and claim duration.
http://dx.doi.org.libproxy.lib.unc.edu/10.1136/bmjopen-2015-007836 Busse JW, Ebrahim S, Heels-Ansdell D, Wang L, Couban R, Walter SD. Association of worker characteristics and early reimbursement for physical therapy, chiropractic and opioid prescriptions with workers’ compensation claim duration, for cases of acute low back pain: an observational cohort study. BMJ Open. 2015;5(8):e007836. doi:10.1136/bmjopen-2015-007836.
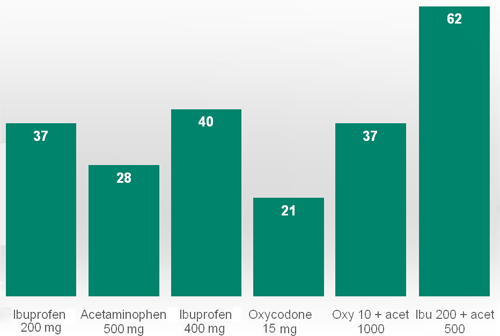
Efficacy of pain medications
Acute pain26,27
Percent with 50% pain relief
Chronic pain
No evidence that opioids are effective for long-term treatment of chronic pain.30
Epidemiologic studies have shown that those on chronic opioid therapy have worse quality of life than those with chronic pain who are not.31
The AAN recommends against using opioids for back pain, headaches, or fibromyalgia.36
Treatment of Opioid Use Disorder
- Detox and abstinence: Success rate ≈ 10%
- Methadone: Success rate ≈ 60%
- Buprenorphine (Suboxone®) : Success rate ≈ 60%
- Naltrexone injection (Vivitrol®) : Success rate ≈ 10%
Six things you can do...
- Review your Drug Free Workplace written policy.
- Educate employees.
- Supervise training.
- Enhance your drug testing protocols.
- Educate your doctors and providers.
- Utilize your EAP
1. Review your Drug Free Workplace written policy
- Statement regarding the purpose of a DFWP policy: Safety and health of employees.
- Many samples available on the internet. It is probably best to hire an expert or an organization who specializes in this.
- Make sure you identify safety-sensitive positions.
- State that opioids and other impairing substances cannot be taken by employees in these positions!
- Identify policy for positive drug tests.
2. Educate employees
- Safety talks, posters, flyers, etc. to educate them on the dangers of opioid pain medications.
- Employees must also know the drug-free workplace policy.
- They should know the ramifications of a positive test.
- This also gives you the opportunity to educate them on the dangers of prescription drugs.
- Help them to understand that drug testing is meant to help them:
- It identifies those with the disease of addiction.
- It prevents addiction by reducing recreational drug use.
3. Supervisor training
- They must know the drug-free workplace policy
- They must know what should trigger “reasonable suspicion” testing
- Requesting a drug test should not be punitive.
Reasonable suspicion
- Odd behavior
- Less punctual
- Increased absences
- Decrease work quality/effectiveness
- eports from other employees
- Reports or witnessed behavior in the community
4. Drug testing
Keys:
- Know the drugs that are used in your area
- Make sure you are testing for them!
- Do not just accept a 5-panel or 10-panel test.
- Work with your Medical Review Officer.
- If a test is positive, it should be reported to you even if there is a legitimate prescription!
- Test at the right times.
- Random, post-accident, return to work, while in treatment, reasonable suspicion.
SAMHSA5
Testing conducted according to SAMHSA’s guidelines checks for five illicit drugs plus, in some cases, alcohol (ethanol, ethyl alcohol, booze). These five illicit drugs are:
- Amphetamines (Adderall, meth, speed, crank, ecstasy)
- THC (cannabinoids, marijuana, hash)
- Cocaine (coke, crack)
- Opiates (heroin, codeine, morphine, maybe hydrocodone)
- Phencyclidine (PCP, angel dust)
Additional tests
- Oxycodone
- Methadone
- Benzodiazepines
- Fentanyl?
5. Educate your doctors/providers
- Opioids are no more effective than ibuprofen-type drugs for treatment of acute and chronic pain.
- Opioids have more side-effects.
- Opioids lead to worse outcomes and higher costs.
- Opioids should never be used for acute back pain.
- Multidisciplinary approach may be needed.
- Return to work ASAP.
6. Employee Assistance Programs (EAPs)
- Make sure you have a decent EAP provider. If they don’t do assessment and or treatment of substance abuse, make sure they have access to someone who does.
- **Opioid abuse/dependence is a special creature and needs special treatment. Make sure your EAP can provide (or refer to) medication assisted treatment!
- Addiction is a DISEASE!!! It is treatable. Workplace referrals for treatment save lives!
Review
- Review your Drug Free Workplace written policy
- Educate employees
- Supervisor training
- Drug testing
- Educate your doctors/providers
- Employee Assistance Programs (EAPs)
Resources
https://www.samhsa.gov/workplace
http://www.generationrxworkplace.com/index.html
http://safety.nsc.org/rxemployerkit
References
1. Solanki DR, Koyyalagunta D, Shah R V, Silverman SM, Manchikanti L. Monitoring opioid adherence in chronic pain patients: assessment of risk of substance misuse. Pain Physician. 2011;14(2):E119-E131. http://www.ncbi.nlm.nih.gov/pubmed/21412377.
2. Seya M-J, Gelders SF a M, Achara OU, Milani B, Scholten WK. A first comparison between the consumption of and the need for opioid analgesics at country, regional, and global levels. J Pain Palliat Care Pharmacother. 2011;25(1):6-18. doi:10.3109/15360288.2010.536307.
3. NIDA. Safe Prescribing for Pain. 2016. https://www.drugabuse.gov/nidamed/etools/safe-prescribing-pain.
4. Paulozzi LJ, Baldwin G. CDC Grand Rounds: Prescription Drug Overdoses — a U.S. Epidemic. MMWR. 2012;61(1):10-13.
5. Murray C. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591-608. doi:10.1001/jama.2013.13805.
6. Birnbaum HG, White AG, Schiller M, Waldman T, Cleveland JM, Roland CL. Societal Costs of Prescription Opioid Abuse , Dependence , and Misuse in the United States. Pain Med. 2011;12:657-667.
7. Paulozzi LJ, Jones CM, Mack KA, Rudd RA. Vital signs: overdoses of prescription opioid pain relievers---United States, 1999--2008. MMWR Morb Mortal Wkly Rep. 2011;60(43):1487-1492. http://www.ncbi.nlm.nih.gov/pubmed/22048730.
8. Cherrier MM, Amory JK, Ersek M, Risler L, Shen DD. Comparative cognitive and subjective side effects of immediate-release oxycodone in healthy middle-aged and older adults. J Pain. 2009;10(10):1038-1050. doi:10.1016/j.jpain.2009.03.017.
9. Gooch CM, Rakitin BC, Cooper ZD, Comer SD, Balsam PD. Oxycodone lengthens reproductions of suprasecond time intervals in human research volunteers. Behav Pharmacol. 2011;22(4):354-361. doi:10.1097/FBP.0b013e328348d8b8.
10. Thiele RH, Rea KM, Turrentine FE, et al. Standardization of Care: Impact of an Enhanced Recovery Protocol on Length of Stay, Complications, and Direct Costs after Colorectal Surgery. J Am Coll Surg. 2015;220(4):430-443. doi:10.1016/j.jamcollsurg.2014.12.042.
11. Woller S a., Hook M a. Opioid administration following spinal cord injury: Implications for pain and locomotor recovery. Exp Neurol. 2013;247:328-341. doi:10.1016/j.expneurol.2013.03.008.
12. White J a, Tao X, Talreja M, Tower J, Bernacki E. The effect of opioid use on workers’ compensation claim cost in the State of Michigan. J Occup Environ Med. 2012;54(8):948-953. doi:10.1097/JOM.0b013e318252249b.
13. Edlund MJ, Martin BC, Russo JE, Devries A, Braden JB, Sullivan MD. The Role of Opioid Prescription in Incident Opioid Abuse and Dependence Among Individuals With Chronic Noncancer Pain. Clin J Pain. 2014;30(7):557-564.
14. Chu LF, Clark DJ, Angst MS. Opioid tolerance and hyperalgesia in chronic pain patients after one month of oral morphine therapy: a preliminary prospective study. J Pain. 2006;7(1):43-48. doi:10.1016/j.jpain.2005.08.001.
15. Webster BS, Verma SK, Gatchel RJ. Relationship between early opioid prescribing for acute occupational low back pain and disability duration, medical costs, subsequent surgery and late opioid use. Spine (Phila Pa 1976). 2007;32(19):2127-2132. doi:10.1097/BRS.0b013e318145a731.
16. Miller M, Stu ÃT, Azrael D. Opioid Analgesics and the Risk of Fractures in Older Adults with Arthritis. J Am Geriatr Soc. 2011;59:430-438. doi:10.1111/j.1532-5415.2011.03318.x.
17. Ray WA, Chung CP, Murray KT, et al. Prescription of Long-Acting Opioids and Mortality in Patients With Chronic Noncancer Pain. JAMA. 2016;315(22):2415. doi:10.1001/jama.2016.7789.
18. Solomon DH, Rassen J a, Glynn RJ, Lee J, Levin R, Schneeweiss S. The comparative safety of analgesics in older adults with arthritis. Arch Intern Med. 2010;170(22):1968-1976. doi:10.1001/archinternmed.2010.391.
19. Tenore PL. Psychotherapeutic benefits of opioid agonist therapy. J Addict Dis. 2008;27(3):49-65. doi:10.1080/10550880802122646.
20. Younger JW, Chu LF, D’Arcy NT, Trott KE, Jastrzab LE, Mackey SC. Prescription opioid analgesics rapidly change the human brain. Pain. 2011;152(8):1803-1810. doi:10.1016/j.pain.2011.03.028.
21. Martell B, O’Connor P, Kerns R, et al. Systematic review: opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Ann Intern Med. 2007;146(2):116-127. http://annals.org/article.aspx?articleid=732048. Accessed August 9, 2014.
22. Odgers CL, Caspi A, Nagin DS, et al. Is it important to prevent early exposure to drugs and alcohol among adolescents? Psychol Sci. 2008;19(10):1037-1044. doi:10.1111/j.1467-9280.2008.02196.x.
23. Polunina AG, Bryun E a. Neuropsychological Functions of μ- and δ-Opioid Systems. ISRN Addict. 2013;2013:1-13. doi:10.1155/2013/674534.
24. Inagaki TK, Ray LA, Irwin MR, Way BM, Eisenberger NI. Opioids and social bonding: Naltrexone reduces feelings of social connection. Soc Cogn Affect Neurosci. 2016;epub ahead:1-8. doi:10.1093/scan/nsw006.
25. Schweiger D, Stemmler G, Burgdorf C, Wacker J. Opioid receptor blockade and warmth-liking: Effects on interpersonal trust and frontal asymmetry. Soc Cogn Affect Neurosci. 2014;9(10):1608-1615. doi:10.1093/scan/nst152.
26. Teater D. Evidence for the Efficacy of Pain Medications. Itasca, Illinois; 2014. www.nsc.org/painmedevidence.
27. Moore RA, Derry S, McQuay HJ, Wiffen PJ. Single dose oral analgesics for acute postoperative pain in adults. Cochrane Database Syst Rev. 2011;9(9):CD008659. doi:10.1002/14651858.CD008659.pub2.
28. Holdgate A, Pollock T. Nonsteroidal anti-inflammatory drugs ( NSAIDs ) versus opioids for acute renal colic. Cochrane Database Syst Rev. 2004;(1):Art. No.: CD004137. doi:10.1002/14651858.CD004137.pub3.
29. Kleinert R, Lange C, Steup A, Black P, Goldberg J, Desjardins P. Single dose analgesic efficacy of tapentadol in postsurgical dental pain: The results of a randomized, double-blind, placebo-controlled study. Anesth Analg. 2008;107(6):2048-2055. doi:10.1213/ane.0b013e31818881ca.
30. Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain — United States, 2016. MMWR. 2016;65. doi:10.1001/jama.2016.1464.
31. Eriksen J, Sjøgren P, Bruera E, Ekholm O, Rasmussen NK. Critical issues on opioids in chronic non-cancer pain: an epidemiological study. Pain. 2006;125(1-2):172-179. doi:10.1016/j.pain.2006.06.009.
32. Afilalo M, Etropolski MS, Kuperwasser B, et al. Efficacy and Safety of Tapentadol Extended Release Compared with Oxycodone Controlled Release for the Management of Moderate to Severe Chronic Pain Related to Osteoarthritis of the Knee: A Randomized, Double-Blind, Placebo- and Active-Controlled Phase III. Clin Drug Investig. 2010;30(8):489-505. doi:1 [pii]\n10.2165/11533440-000000000-00000.
33. Cherkin DC, Sherman KJ, Balderson BH, et al. Effect of Mindfulness-Based Stress Reduction vs Cognitive Behavioral Therapy or Usual Care on Back Pain and Functional Limitations in Adults With Chronic Low Back Pain. JAMA. 2016;315(12):1240. doi:10.1001/jama.2016.2323.
34. Krumova EK, Bennemann P, Kindler D, Schwarzer A, Zenz M, Maier C. Low pain intensity after opioid withdrawal as a first step of a comprehensive pain rehabilitation program predicts long-term nonuse of opioids in chronic noncancer pain. Clin J Pain. 2013;29(9):760-769. doi:10.1097/AJP.0b013e31827c7cf6.
35. Darchuk KM, Townsend CO, Rome JD, Bruce BK, Hooten WM. Longitudinal treatment outcomes for geriatric patients with chronic non-cancer pain at an interdisciplinary pain rehabilitation program. Pain Med. 2010;11(9):1352-1364. doi:10.1111/j.1526-4637.2010.00937.x.
36. da Costa B, Nüesch E, Aws R, et al. Oral or transdermal opioids for osteoarthritis of the knee or hip ( Review ) Oral or transdermal opioids for osteoarthritis of the knee or hip. Cochrane Database Syst Rev. 2014;(9). doi:10.1002/14651858.CD003115.pub3.Copyright.
37. Franklin GM. Opioids for chronic noncancer pain: a position paper of the American Academy of Neurology. Neurology. 2014;83(14):1277-1284. doi:10.1212/WNL.0000000000000839.
38. Balague F, Mannion AF, Pellise F, Cedraschi C. Non-specific low back pain. Lancet. 2012;379(9814):482-491. doi:10.1016/S0140-6736(11)60610-7.
39. Artus M, van der Windt DA, Jordan KP, Hay EM. Low back pain symptoms show a similar pattern of improvement following a wide range of primary care treatments: A systematic review of randomized clinical trials. Rheumatology. 2010;49(12):2346-2356. doi:10.1093/rheumatology/keq245.
40. Cherkin DC, Sherman KJ, Balderson BH, et al. Effect of Mindfulness-Based Stress Reduction vs Cognitive Behavioral Therapy or Usual Care on Back Pain and Functional Limitations in Adults With Chronic Low Back Pain. JAMA. 2016;315(12):1240. doi:10.1001/jama.2016.2323.
41. Webster BS, Verma SK, Gatchel RJ. Relationship between early opioid prescribing for acute occupational low back pain and disability duration, medical costs, subsequent surgery and late opioid use. Spine (Phila Pa 1976). 2007;32(19):2127-2132. doi:10.1097/BRS.0b013e318145a731.
42. Franklin GM, Stover BD, Turner J a, Fulton-Kehoe D, Wickizer TM. Early opioid prescription and subsequent disability among workers with back injuries: the Disability Risk Identification Study Cohort. Spine (Phila Pa 1976). 2008;33(2):199-204. doi:10.1097/BRS.0b013e318160455c.
43. Edlund MJ, Martin BC, Russo JE, Devries A, Braden JB, Sullivan MD. The Role of Opioid Prescription in Incident Opioid Abuse and Dependence Among Individuals With Chronic Noncancer Pain. Clin J Pain. 2014;30(7):557-564.
44. Lee D, Armaghani S, Archer KR, et al. Preoperative Opioid Use as a Predictor of Adverse Postoperative Self-Reported Outcomes in Patients Undergoing Spine Surgery. J Bone Jt Surg. 2014;96(11):e89-e89. doi:10.2106/JBJS.M.00865.
45. Shaheed CA, Maher CG, Williams KA, Day R, Mclachlan AJ. Efficacy, Tolerability, and Dose-Dependent Effects of Opioid Analgesics for Low Back Pain A Systematic Review and Meta-analysis. JAMA Intern Med. 2016;176(7):958-968. doi:10.1001/jamainternmed.2016.1251.
46. Eriksen J, Sjøgren P, Bruera E, Ekholm O, Rasmussen NK. Critical issues on opioids in chronic non-cancer pain: an epidemiological study. Pain. 2006;125(1-2):172-179. doi:10.1016/j.pain.2006.06.009.