Overlapping Vulnerabilities: The Occupational Health and Safety of Young Immigrant Workers in Small Construction Firms
Summary Statement
The American Society of Safety Engineers (ASSE) and the National Institute for Occupational Safety and Health (NIOSH) joined forces to produce this report as part of a national outreach effort. This document focuses on three populations that have been shown to be at increased risk for adverse work-related health outcomes—Hispanic immigrants, small business employees, and workers under 25 years old, with a specific focus on implications for the construction industry. It explores how the combination of risk factors may result in overlapping vulnerabilities for workers such as young immigrants in small construction firms and
discusses the implications for OSH professionals.
May 2015
NIOSH and ASSE Report • May 2015
DHHS (NIOSH) Publication No. 2015–178

This document is in the public domain and may be freely copied or reprinted.
Acknowledgements
This report was created by scientists and staff of the National Institute for Occupational Safety and Health (NIOSH) and the American Society for Safety Engineers (ASSE). The authors thank Paula Leite and her team at the Center for Migration Studies of the Mexican Ministry of Governance for their assistance with the data from the Border Survey of Mexican Migration, or EMIF Norte. They also thank Sue Dong and Eileen Betit, of The Center for Construction Research and Training, for their help in defining the size of the construction worker population with overlapping vulnerabilities and for their previous efforts at tailoring interventions for these workers. The authors also thank Alberto J. Caban-Martinez of the University of Miami Leonard E. Miller School of Medicine for his help with compiling and analyzing the data from the National Health Interview Survey. Seleen Collins provided editorial support, and Vanessa Williams contributed to the design and layout of this document.
The following external peer reviewers provided comments on a draft of this report:
- Eileen Betit, Director, Research to Practice (r2p),
CPWR-The Center for Construction Research and Training - Oscar Chacon, Executive Director,
National Alliance of Latin American and Caribbean Communities - Charlotte Chang, DrPH, Coordinator of Research to Practice and Evaluation,
University of California, Berkeley - Ann Marie Dale, PhD, Assistant Professor of Medicine and Occupational Therapy,
Washington University - Sue Dong, DrPH, Data Center Director,
CPWR-The Center for Construction Research and Training - Diane Rohlman, PhD, Associate Professor,
Iowa University - Scott Schneider, MS, CIH, Director,
Occupational Safety and Health Laborers’ Health and Safety Fund of North America - Amy Shannon, MBA, Senior Advisor,
National Alliance of Latin American and Caribbean Communities
Contents
- Executive Summary
- 1. Introduction
- 2. Overlapping Vulnerabilities in the Construction Sector
- 3. Characteristics of Selected Vulnerable Populations in the Construction Industry
- 4. Size of the Vulnerable Population
- 5. Conceptualizing Overlapping Vulnerabilities and Their Interaction
- 6. Interventions that Address OSH Vulnerabilities
- 7. How OSH Interventions May Address Multiple Vulnerabilities
- 8. Endnotes and References
- Disclaimer, Ordering Information, Suggested Citation
Executive Summary
 The American Society of Safety Engineers (ASSE) and the National Institute for Occupational Safety and Health (NIOSH) are the initiators of an intervention effort to reach workers experiencing overlapping occupational safety and health (OSH) vulnerabilities in small construction businesses. This report focuses on three populations that research indicates are at increased risk for adverse work-related health outcomes—Hispanic immigrants (individuals born in Latin America who currently live in the United States), small business employees (firms with fewer than 20 employees), and young workers (<25 years old)—with a specific focus on implications for the construction industry. It explores how the combination of risk factors may result in overlapping vulnerabilities for workers such as young immigrants in small construction firms and discusses the implications for OSH professionals.
The American Society of Safety Engineers (ASSE) and the National Institute for Occupational Safety and Health (NIOSH) are the initiators of an intervention effort to reach workers experiencing overlapping occupational safety and health (OSH) vulnerabilities in small construction businesses. This report focuses on three populations that research indicates are at increased risk for adverse work-related health outcomes—Hispanic immigrants (individuals born in Latin America who currently live in the United States), small business employees (firms with fewer than 20 employees), and young workers (<25 years old)—with a specific focus on implications for the construction industry. It explores how the combination of risk factors may result in overlapping vulnerabilities for workers such as young immigrants in small construction firms and discusses the implications for OSH professionals.
Social dynamics such as race, class, and gender; economic trends such as the growth of the temporary workforce; and organizational factors such as business size can all contribute to the greater vulnerability of some workers to workplace illness or injury than others. OSH professionals will be better able to effectively assist in protecting workers if they are aware of and account for these factors when they design and implement safety programs and OSH interventions.
This report first explores the demographic trends associated with each of these vulnerable groups of workers. Next, the current OSH literature is explored to determine the extent to which these risk factors are being examined in combination with each other. A conceptual model is then presented for understanding how the vulnerabilities interact when a worker belongs to all three groups. The report concludes by considering the efforts needed to address and reduce the pervasive and persistent occupational health disparities experienced by vulnerable workers:
- Evaluating the potential overlap and interaction of different vulnerabilities
- Developing interventions tailored to all relevant vulnerabilities
- Working with organizations known to the target community, for effective diffusion of interventions
- Building relationships between OSH professionals and community organizations and focusing on the sustainability of interventions.
1. Introduction
 Not all workers have the same risk of being injured at work, even when they are in the same industry or have the same job. In addition to differential hazard exposure, other factors can make some workers more vulnerable than others to workplace illness or injury. These include social dynamics such as race, class, and gender; economic trends such as the growth of the temporary workforce; and organizational factors such as business size. Occupational safety and health (OSH) professionals will be better able to effectively assist in protecting workers if they are aware of and account for these factors when they design and implement safety programs and interventions.
Not all workers have the same risk of being injured at work, even when they are in the same industry or have the same job. In addition to differential hazard exposure, other factors can make some workers more vulnerable than others to workplace illness or injury. These include social dynamics such as race, class, and gender; economic trends such as the growth of the temporary workforce; and organizational factors such as business size. Occupational safety and health (OSH) professionals will be better able to effectively assist in protecting workers if they are aware of and account for these factors when they design and implement safety programs and interventions.
The term occupational health disparities refers to increased rates of work-related illness and injuries in particularly vulnerable populations [Centers for Disease Control and Prevention (CDC), 2011]. Vulnerable populations are often described using a single characteristic (age, race, income, employment, etc.) [Cutter et al. 2005]. A growing body of research explores how a particular characteristic, such as being an immigrant, a racial minority, or a temporary worker, can increase an individual’s risk for occupational injury or illness and suggests effective ways to improve their safety and health. OSH professionals have benefitted from this research in being better able to serve certain vulnerable groups, such as providing Hispanic immigrants with training materials in the Spanish language. However, as occupational health disparities research demonstrates, workers frequently belong to more than one of these vulnerable groups that affect their overall risk of injury or fatality [Krieger 2010]. Young Hispanic immigrant workers are never singularly Hispanic one day, immigrants the next day, and young persons the following day; they are all of these every day. As such, they embody the vulnerabilities associated with these characteristics, all at the same time. Practitioners and researchers often address these characteristics in isolation rather than in combination because of several factors, such as (1) the limitations of data sets used for occupational epidemiology [Souza et al. 2010]; (2) the important yet limited scientific approach of understanding the impact of each factor by studying it independently; and (3) the practical and immediate demands on practitioners (for example, overcoming language differences to get the job done safely and on time). The purpose of this report is to explore this combination of risk factors, or overlapping vulnerabilities, and to describe their implications for OSH professional practice.
 A worker with overlapping vulnerabilities is simultaneously a member of two or more at-risk groups such as immigrants, temporary workers, new workers, older workers, small business employees, and non-union workers. Each vulnerability has characteristics that add unique barriers to the worker’s OSH (for example, an immigrant worker’s fear of deportation for reporting unsafe conditions) [Flynn 2010] or that intensify existing barriers to safety that are common for all workers (such as lack of training in small businesses due to financial constraints) [Cunningham et al. 2014]. As these vulnerabilities are independently associated with additional risk of workplace injury or illness, the interaction between risk factors may create even more risk for groups experiencing multiple vulnerabilities than for those who have only one risk factor. However, more work is needed to clarify how these overlapping vulnerabilities interact and may intensify the risk for occupational injury and illness and how OSH professionals can effectively reduce these risks.
A worker with overlapping vulnerabilities is simultaneously a member of two or more at-risk groups such as immigrants, temporary workers, new workers, older workers, small business employees, and non-union workers. Each vulnerability has characteristics that add unique barriers to the worker’s OSH (for example, an immigrant worker’s fear of deportation for reporting unsafe conditions) [Flynn 2010] or that intensify existing barriers to safety that are common for all workers (such as lack of training in small businesses due to financial constraints) [Cunningham et al. 2014]. As these vulnerabilities are independently associated with additional risk of workplace injury or illness, the interaction between risk factors may create even more risk for groups experiencing multiple vulnerabilities than for those who have only one risk factor. However, more work is needed to clarify how these overlapping vulnerabilities interact and may intensify the risk for occupational injury and illness and how OSH professionals can effectively reduce these risks.
 To illustrate the concept of overlapping vulnerabilities, this report focuses on three populations that research indicates are at increased risk for adverse work-related health outcomes— Hispanic immigrants (individuals living in the United States who were born in Latin America), small business employees (firms with fewer than 20 employees), and young workers (< 25 years old) —with a specific focus on implications for those in the construction industry. First, the report explores the demographic trends associated with these vulnerable groups across all industries and, specifically, as they relate to these groups in the construction sector. Next, it analyzes the current safety and health literature to determine the extent to which these vulnerabilities are being studied in combination with each other. Although the vulnerabilities explored here are not the only ones faced by the U.S. working population, they are of specific concern to the construction industry, where Hispanic immigrant workers, young workers, and small business employees have each been shown to be at increased risk for occupational injury and illness relative to other workers. This report also presents a conceptual model of how the vulnerabilities interact for individuals belonging to all three groups. Finally, it offers suggestions to address and reduce the pervasive, persistent occupational health disparities among vulnerable workers in construction.
To illustrate the concept of overlapping vulnerabilities, this report focuses on three populations that research indicates are at increased risk for adverse work-related health outcomes— Hispanic immigrants (individuals living in the United States who were born in Latin America), small business employees (firms with fewer than 20 employees), and young workers (< 25 years old) —with a specific focus on implications for those in the construction industry. First, the report explores the demographic trends associated with these vulnerable groups across all industries and, specifically, as they relate to these groups in the construction sector. Next, it analyzes the current safety and health literature to determine the extent to which these vulnerabilities are being studied in combination with each other. Although the vulnerabilities explored here are not the only ones faced by the U.S. working population, they are of specific concern to the construction industry, where Hispanic immigrant workers, young workers, and small business employees have each been shown to be at increased risk for occupational injury and illness relative to other workers. This report also presents a conceptual model of how the vulnerabilities interact for individuals belonging to all three groups. Finally, it offers suggestions to address and reduce the pervasive, persistent occupational health disparities among vulnerable workers in construction.
2. Overlapping Vulnerabilities in the Construction Sector
 The concept of examining multiple occupational risk factors in this context is not new. One example explores the confluence of multiple social vulnerabilities in OSH outcomes by using data from the Census of Fatal Occupational Injuries, 2005–2009 [Steege et al. 2014]. Findings indicate that the rate of fatal occupational injuries for foreign-born workers of all ages was 4.0 per 100,000, versus 3.7 per 100,000 for all workers. “Foreign born” refers to nativity status and is defined as persons not born in the U.S. or its territories [Steege et al. 2014]. Furthermore, the rates for young foreign-born workers were even higher, particularly for the youngest workers (4.8 per 100,000 for those aged 20–24 years and 6.1 for those aged 15–19 years). These data suggest that the vulnerability associated with being a foreign-born worker interacted with the vulnerabilities associated with being a young worker, creating an elevated risk for fatal occupational injuries. What is unclear from the data is which of the barriers to safety for each of these groups were central to this increased fatality rate, how they interacted to put young foreign-born workers at an increased risk, and how to best tailor interventions to reduce this additional risk. These are all questions that warrant further study. However, OSH professionals and programs can immediately begin to work on finding ways to effectively assist workers who are in overlapping vulnerable populations.
The concept of examining multiple occupational risk factors in this context is not new. One example explores the confluence of multiple social vulnerabilities in OSH outcomes by using data from the Census of Fatal Occupational Injuries, 2005–2009 [Steege et al. 2014]. Findings indicate that the rate of fatal occupational injuries for foreign-born workers of all ages was 4.0 per 100,000, versus 3.7 per 100,000 for all workers. “Foreign born” refers to nativity status and is defined as persons not born in the U.S. or its territories [Steege et al. 2014]. Furthermore, the rates for young foreign-born workers were even higher, particularly for the youngest workers (4.8 per 100,000 for those aged 20–24 years and 6.1 for those aged 15–19 years). These data suggest that the vulnerability associated with being a foreign-born worker interacted with the vulnerabilities associated with being a young worker, creating an elevated risk for fatal occupational injuries. What is unclear from the data is which of the barriers to safety for each of these groups were central to this increased fatality rate, how they interacted to put young foreign-born workers at an increased risk, and how to best tailor interventions to reduce this additional risk. These are all questions that warrant further study. However, OSH professionals and programs can immediately begin to work on finding ways to effectively assist workers who are in overlapping vulnerable populations.
The next section explores the overlap of occupational health disparities of Hispanic immigrants, employees of small businesses, and young workers in the construction industry. Unfortunately, there are relatively few data sources that include the necessary detail to identify overlapping OSH vulnerabilities among young immigrant workers and small business employees. For this analysis, a “young worker” is defined as one under the age of 25, a “small business” is defined as one with 20 or fewer employees, and a “very small business” is defined as one with fewer than 10 employees, on the basis of the data ranges used. This report suggests the importance of understanding how the vulnerabilities for occupational injury associated with being a Hispanic immigrant, young worker, and employee of a small business may overlap in the construction industry, and how these different vulnerabilities may manifest themselves, interact with, and build on one another in the lived experience of individual workers—as illustrated in Case Studies 1 to 3.
Understanding the role overlapping vulnerabilities play in occupational health disparities requires work in at least four areas:
- Identifying the vulnerable populations and the associated characteristics related to OSH
- Determining the size of the population that shares more than one vulnerability and assessing their risk for occupational injury and illness relative to their counter parts
- Exploring how the vulnerabilities associated with these characteristics may interact with one another or increase the risk for injury on the job
- Designing effective interventions to reduce the occupational health disparities associated with them.
3. Characteristics of Selected Vulnerable Populations in the Construction Industry
3.1 Hispanic Immigrants
 The Hispanic population in the United States has grown substantially in recent years. Currently, more than 50 million Hispanics live in this country, comprising roughly 16% of the total U.S. population and about 14% of the total U.S. workforce [U.S. Census Bureau 2014a]. In 2013, immigrants comprised half of the 22 million Hispanics employed in the United States [Kochhar 2014]. Approximately 5% of the U.S. workforce is composed of undocumented Hispanic immigrants [Passel et al. 2011]. The Pew Hispanic Center [2008] estimated that immigrants will comprise approximately a quarter of the U.S. working population by 2050. It is also predicted that immigrants and their children will account for 83% of the growth in the working-age population of the United States during this same period [Congressional Budget Office 2005]. Unique challenges for employers and OSH professionals are likely to arise as a result of this steady influx of immigrants into the U.S. workforce.
The Hispanic population in the United States has grown substantially in recent years. Currently, more than 50 million Hispanics live in this country, comprising roughly 16% of the total U.S. population and about 14% of the total U.S. workforce [U.S. Census Bureau 2014a]. In 2013, immigrants comprised half of the 22 million Hispanics employed in the United States [Kochhar 2014]. Approximately 5% of the U.S. workforce is composed of undocumented Hispanic immigrants [Passel et al. 2011]. The Pew Hispanic Center [2008] estimated that immigrants will comprise approximately a quarter of the U.S. working population by 2050. It is also predicted that immigrants and their children will account for 83% of the growth in the working-age population of the United States during this same period [Congressional Budget Office 2005]. Unique challenges for employers and OSH professionals are likely to arise as a result of this steady influx of immigrants into the U.S. workforce.
 Hispanic immigrant workers endure a higher burden of occupational injury and fatality than do U.S.-born Hispanic, non-Hispanic, and non-immigrant workers [CDC 2008]. Immigrants often work in “3D” (dirty, dangerous, and demeaning) jobs [Connell 1993] and jobs considered to be high risk [Baron et al. 2013]. Because of their work in dangerous occupations (among other factors), Hispanic immigrant workers experience a higher occupational mortality rate (5.9 per 100,000 full-time-equivalent workers, or FTEs) than all other workers (4.0 per 100,000 FTEs) [CDC 2008], and they were the only racial/ethnic group with an increase in number of workplace fatalities in 2013 [Bureau of Labor Statistics (BLS) 2014e].
Hispanic immigrant workers endure a higher burden of occupational injury and fatality than do U.S.-born Hispanic, non-Hispanic, and non-immigrant workers [CDC 2008]. Immigrants often work in “3D” (dirty, dangerous, and demeaning) jobs [Connell 1993] and jobs considered to be high risk [Baron et al. 2013]. Because of their work in dangerous occupations (among other factors), Hispanic immigrant workers experience a higher occupational mortality rate (5.9 per 100,000 full-time-equivalent workers, or FTEs) than all other workers (4.0 per 100,000 FTEs) [CDC 2008], and they were the only racial/ethnic group with an increase in number of workplace fatalities in 2013 [Bureau of Labor Statistics (BLS) 2014e].
3.1.1 Hispanic Immigrant Workers in Construction
One high-risk industry with a high concentration of Hispanic immigrant workers is construction. In 2013, Hispanic immigrants accounted for approximately 20% (1,798,192) of the construction workforce (9,106,227) in the United States and 75% of all Hispanics (2,379,323) working in this industry were immigrants [U.S. Census Bureau 2014b]. The rapid growth in the number of Hispanic immigrant workers in the construction industry has been accompanied by increased numbers of occupational injuries. The number of cases of nonfatal injury or illness among Hispanic construction workers nearly doubled (from 17,715 to 33,930) from 1992 to 2006 [Dong et al. 2010]. From 2003 to 2008, the occupation groups with the highest fatality rate for Hispanic construction workers were ironworkers (135 deaths per 100,000 FTEs), roofers (28 deaths per 100,000 FTEs), and laborers (22 deaths per 100,000 FTEs).
3.1.2 Reasons for Disparities
 A multitude of knowledge, cultural, and structural barriers contribute to the disparity in occupational injury experienced by Hispanic immigrants. Many immigrants are unfamiliar with the risks they face on the job, standard safety procedures in the United States, and the regulatory infrastructure that protects their right to a safe workplace [Flynn 2014]. Therefore, workplace safety training is critical. However, immigrant workers frequently report not receiving any safety training on the job or receiving poor quality training [O’Connor et al. 2005]. Furthermore, language differences among immigrant workers, their supervisors, and coworkers are one of the most frequently cited barriers to safety [Gany et al. 2011]. In addition, cultural factors, such as how immigrants understand and approach work, safety, risk, and their relationship with their coworkers and employers, also contribute to OSH disparities among workers in this population. For example, a study of Hispanic immigrant workers in Chicago showed that workers’ behaviors reflected a culture that placed a high value on being perceived as hard workers by their employer [Gomberg-Muñoz 2010]. This cultural value increased their likelihood of taking risks, such as working too fast. Structural barriers— including global pressure on production and wages [Siqueira et al. 2014], racism [Okechukwu et al. 2014; Krieger et al. 2006], and industry practices, such as a growing reliance on temporary workers [Landsbergis et al. 2014]—further exacerbate occupational health disparities among Hispanic worker populations in this country.
A multitude of knowledge, cultural, and structural barriers contribute to the disparity in occupational injury experienced by Hispanic immigrants. Many immigrants are unfamiliar with the risks they face on the job, standard safety procedures in the United States, and the regulatory infrastructure that protects their right to a safe workplace [Flynn 2014]. Therefore, workplace safety training is critical. However, immigrant workers frequently report not receiving any safety training on the job or receiving poor quality training [O’Connor et al. 2005]. Furthermore, language differences among immigrant workers, their supervisors, and coworkers are one of the most frequently cited barriers to safety [Gany et al. 2011]. In addition, cultural factors, such as how immigrants understand and approach work, safety, risk, and their relationship with their coworkers and employers, also contribute to OSH disparities among workers in this population. For example, a study of Hispanic immigrant workers in Chicago showed that workers’ behaviors reflected a culture that placed a high value on being perceived as hard workers by their employer [Gomberg-Muñoz 2010]. This cultural value increased their likelihood of taking risks, such as working too fast. Structural barriers— including global pressure on production and wages [Siqueira et al. 2014], racism [Okechukwu et al. 2014; Krieger et al. 2006], and industry practices, such as a growing reliance on temporary workers [Landsbergis et al. 2014]—further exacerbate occupational health disparities among Hispanic worker populations in this country.
3.2 Small Business
In 2010, firms with fewer than 500 workers accounted for 99.7% of all businesses in the United States, and businesses with fewer than 20 workers accounted for 89.8% of the total number of firms [U.S. Census Bureau 2011]. Although the definition of a “small” business varies widely, particularly as it relates to discussions of OSH, the characteristics that distinguish a smaller business from a larger one in terms of OSH capacities include not only number of employees, but also the structure (including sole proprietorships), the age of the business (most new businesses are small), and a manager-centered culture (the owner/operator sets the culture of the business) [Cunningham et al. 2014]. Thus, what is considered a small business may vary across industries, and businesses with 20 or fewer employees tend to fit these characteristics in construction. Smaller firms provide the U.S. economy with more net new jobs than larger ones [Headd 2010], and a long-term downward trend in U.S. business size is expected [Choi and Spletzer 2012].
 Evidence suggests that smaller businesses experience a disproportionate burden of occupational injuries, illnesses, and fatalities. Previous research has found that employees from smaller businesses may face increased exposure to physical hazards [Morse et al. 2004], and numerous studies report a linear, inverse relationship between organization size and reports of injury, illness, and/or fatality [Buckley et al. 2008; Fabiano et al. 2004; Fenn and Ashby 2004; Jeong 1998; Mendeloff et al. 2006; Morse et al. 2004; Page 2009; Peek-Asa et al. 1999], as well as an association with longer duration of work-related disability [Cheadle et al. 1994; Stover et al. 2007]. Many small businesses are exempt from Occupational Safety and Health Administration (OSHA) reporting regulations, which are, for the most part, not required for companies with 10 or fewer employees (with some exceptions, including in the case of a fatal incident) [OSHA 2014]. Small businesses are also more likely than larger businesses to hire workers who are at a greater risk for occupational injury, including young workers, people who are less educated, and immigrants [Belman and Levine 2004].
Evidence suggests that smaller businesses experience a disproportionate burden of occupational injuries, illnesses, and fatalities. Previous research has found that employees from smaller businesses may face increased exposure to physical hazards [Morse et al. 2004], and numerous studies report a linear, inverse relationship between organization size and reports of injury, illness, and/or fatality [Buckley et al. 2008; Fabiano et al. 2004; Fenn and Ashby 2004; Jeong 1998; Mendeloff et al. 2006; Morse et al. 2004; Page 2009; Peek-Asa et al. 1999], as well as an association with longer duration of work-related disability [Cheadle et al. 1994; Stover et al. 2007]. Many small businesses are exempt from Occupational Safety and Health Administration (OSHA) reporting regulations, which are, for the most part, not required for companies with 10 or fewer employees (with some exceptions, including in the case of a fatal incident) [OSHA 2014]. Small businesses are also more likely than larger businesses to hire workers who are at a greater risk for occupational injury, including young workers, people who are less educated, and immigrants [Belman and Levine 2004].
The age of a business can also present OSH challenges. Small businesses in high-risk industries such as construction and forestry that failed after one to two years had an average injury rate about 2.5 times higher (9.7 per 100 full-time employees) than successful companies (3.9) [Holizki et al. 2006]. Although it is unclear precisely why businesses with higher injury rates fail, it may be that an injury results in a loss of business continuity, which leads to business failure [Holizki et al. 2006].
3.2.1 Small Business in Construction
Approximately 90% of construction businesses employ 20 or fewer workers [BLS 2006; Wojcik, et al. 2003; CPWR 2013], and the burden of occupational injury is increased for small construction firms. From 1992 to 2010, 44% (5,893) of construction workers who died as a result of injuries sustained while working were employed by companies with 10 or fewer employees [CPWR 2013]. Trenching and excavation appear to be particularly hazardous activities for small businesses: approximately half (48%) of trenching and excavation fatalities occurred in companies with fewer than 10 employees, and 70% of the fatalities occurred in companies with fewer than 50 workers [CDC 2004].
3.2.2 Reasons for Disparities
The burden of occupational injury faced by small businesses is largely related to knowledge and capacity. Workers who feel that they are already knowledgeable about safety and who have concerns about the credibility of outside safety trainers may experience barriers to being properly trained [Hung et al. 2013]. Small business owners also demonstrate a lack of OSH knowledge by having no return-to-work policies, poor post-injury administration, no safety training, and a lack of clear management guidance [Eakin and MacEachen 1998; Eakin et al. 2010; Huang et al. 2006].
Fewer than 20% of small business owners belong to trade associations, which are a potential source for OSH resources [Gillen et al. 2004]. Small businesses are less likely to focus on activities that are not directly production-related [Page 2009] and are less likely to utilize formal training methods, which are often perceived as costly and time-consuming [Kotey and Folker 2007]. A national survey of companies with fewer than 250 employees found that 87% did not have a safety committee and 87% had not used a safety consultant in the past five years [Dennis 2002]. Furthermore, smaller businesses are less likely to employ on-site safety and health personnel, thereby limiting access to crucial safety assistance [Pedersen and Sieber 1988], and tend to experience higher rates of employee turnover [Hope and Mackin 2007].
3.3 Young Workers
Approximately 18.1 million workers in the United States were aged 16 to 24 in 2013, representing 13% of the workforce [NIOSH 2015]. Nearly 80% of young people work while still in high school [BLS 2005], and the proportion of working adolescents is relatively high when compared with that in other developed countries [National Research Council (NRC) 1998]. Workers younger than age 18—often referred to as adolescent or teen workers—receive special protections under federal and state child labor laws, which identify allowable and prohibited types of work [U.S. Department of Labor (U.S. DOL) 2013; Castillo and Lewko 2013]. The Bureau of Labor Statistics projects that labor force participation for workers aged 16 to 24 years will continue to decline, for a number of reasons. These include greater academic pressure and more educational requirements that have made it more difficult for teens to pursue paid work [Morisi 2008], as well as a decline in real wages that has prompted more young people to pursue educational opportunities [Morisi 2008; Fernandes-Alcantara 2012].
Just as the benefits of work for youth are well documented, so are the risks [Mortimer 2013]. In the United States, young workers suffer disproportionately from workplace injuries. In 2013, 335 workers under 24 years of age died from work-related injuries [BLS 2014d]. During the 10-year period 1998 to 2007, an estimated 7.9 million nonfatal injuries to younger workers were treated in U.S. hospital emergency departments (EDs) [CDC 2010]. The nonfatal injury rate for those aged 15 to 24 was 5.0 ED-treated injuries per 100 FTEs, approximately two times higher than among workers aged 25 or older [CDC 2010]. One study estimated that work-related injuries among youths up to age 19 accounted for an annual cost of $5 billion, or 3.9% of all workplace injury costs in the United States [Miller and Waehrer 1998].
3.3.1 Young Workers in Construction
Federal child labor laws restrict youth under age 16 from working in the construction sector [U.S. DOL 2013]. In 2014 only about 4.6% of youth laborers aged 16 to 24 were employed in construction trades, of which the vast majority (approximately 83%) were between the ages of 20 and 24 [BLS 2014b].
According to 2013 data, the construction industry accounted for 8.8% of injuries and illnesses among workers aged 16 to 24, most of which (roughly 82%) were suffered by youth aged 20 to 24 years [BLS 2014c]. During the period 2003 to 2007, younger workers aged 16 to 24 years in construction had the third highest rate of fatal injury in comparison with those in other industries (10.9 per 100,000 FTEs, versus 36.5 per 100,000 FTEs in mining and 21.3 per 100,000 FTEs in agriculture) [CDC 2010].
Despite special protections for teen workers, young construction workers have reported using equipment or conducting tasks prohibited by federal child labor laws [Rauscher et al. 2012; Runyan et al. 2006]. Young workers who were fatally injured were more likely than adults to be employed at small, nonunion firms, and their employers were more likely to have been cited by OSHA for safety violations [Suruda et al. 2003].
3.3.2 Reasons for Disparities
Although the literature on work-related injuries among adolescents is limited in comparison with that on injuries among adult workers, a substantial base of evidence has been built over the past two decades that identifies both individual factors and work-related factors that increase the risk for job-related injuries among youth. Individual factors including minority status [CDC 2010; Mardis and Pratt 2003], low socioeconomic status [Rauscher and Meyers 2008], and adolescent risk taking and sensation seeking — the desire to pursue novel and intense experiences [Spear 2000; Steinberg 2005; Steinberg et al. 2011]—may increase young people’s likelihood of experiencing a job-related injury [Sudhinaraset and Blum 2010]. Work-related risk factors include fast pace of work [Breslin et al. 2007], inadequate supervision [Runyan et al. 2006; Runyan and Zakocs 2000; Zakocs et al. 1998], equipment use [Knight et al. 1995; Mardis and Pratt 2003], working late, and working with cash and customers [NIOSH 2003; Richardson and Windau 2003; Zierold and Anderson 2006]. Lack of job knowledge and skills, lack of job training, and lack of job control also contribute to heightened risk among younger workers, who might be less likely to recognize hazards, less likely to speak up regarding safety issues [Tucker and Turner 2013], and less aware of their legal rights as workers [NIOSH 2003].
Case Studies
Because it is associated with numerous occupational safety risks, such as falls, equipment malfunctions and/or incidents, and working outdoors in extreme temperatures, construction is one of the most dangerous industries in the United States [Dong et al. 2011]. In 2013, there were 796 fatal on-the-job injuries to workers in the construction industry—more than in any other industry sector and accounting for 18% of all work-related deaths in the United States that year [BLS 2014a]. This industry may be particularly hazardous to vulnerable workers. To demonstrate how the combination of overlapping vulnerabilites of being a Hispanic worker, a young worker, and a small business employee in the construction sector can contribute to devasting results, three case studies involving fatal workplace injuries in the construction industry are presented here.
Case Study 1

Photo 1 (Case Study 1). Location at which the two victims
were buried by the trench collapse. Photo courtesy of county
coroner.
Two brothers, aged 15 and 16, were hired to work on a construction crew doing trench work. They were Hispanic immigrants who had been in the United States for a little over a year and spoke little English. When they applied for the job, they provided false documentation listing both of their ages as 22. The company employed 11 workers at the job site. Once the brothers were hired, they immediately started working and received no orientation or safety training. The crew leader gave instructions in English, which a bilingual employee would translate into Spanish. On their second day of work, as the two were working in the trench (Photo 1), it collapsed on top of them, critically injuring both. Although coworkers uncovered the teens and emergency services arrived quickly, the brothers could not be revived. It is unknown why the youths were in the trench, as the crew leader had not instructed anyone to be in the trench at that time. The brothers’ true ages were not revealed until two days later, when the boys’ parents gave their birth certificates to the funeral director [NIOSH 2004b].
Case Study 2
A 16-year-old Mexican immigrant went to work with his father and uncles at the construction site for a condominium development (see Photograph 2). He was hired by a concrete and framing subcontractor who led a crew of 18 workers. While he was working with his uncle on an elevated work platform (see Photograph 3), the boy fell and hit his head on concrete 10 feet below. His father ran to him from another area of the work site and found him disoriented and unable to walk without support. The project coordinator told the crew leader to take the boy to a nearby hospital, but instead the crew leader took him and his father to a drugstore to buy aspirin and drove them home. By the time the boy’s uncles arrived home that evening, the boy was vomiting and unable to walk. His family took him to the crew leader’s home, and the crew leader drove them to the emergency room. Fearing legal repercussions, the family told emergency room staff that the teenager had hit his head falling off a bicycle. Given the extent of his injuries, the hospital staff doubted that a bike fall was the cause. Within an hour of arriving at the hospital, he died. It took the police a few days to learn that the boy died as a result of a workplace injury. The project coordinator did not find out that his worker had died until four days later, when news reporters arrived at the work site [NIOSH 2004a].

Photo 2 (Case Study 2). This condominium project was the site at which the worker’s fatal fall occurred. Photo by SCOSHA.

Photo 3 (Case Study 2). In this close-up view of the condominium stairwell and balcony area, the black rectangle illustrates the elevated platform, the letter A shows the young worker’s approximate location before falling, and the letter B shows the approximate location of his fall onto concrete, about 10 feet below. Photo by County Coroner’s Office, South Carolina
Case Study 3
An 18-year-old recent Mexican immigrant heard about a construction job from a friend. Although his English was limited and he needed his friend to translate for him, he was hired. The youth did not receive the comprehensive safety training that new employees usually received because the foreman assumed that one of the three project managers provided him with the training. However, each project manager thought the other had trained the new employee. On his second day on the job, the youth was assigned to operate a roller to compact side-by-side plots where the foundation for townhouses would be laid. He was told to observe a coworker on the roller and mimic his movements. While working on an incline where he could not be seen by his friend or supervisors, he was thrown from the operator’s cab and subsequently crushed by the machine. He was not wearing a seatbelt, and the area where he was working had a slope of 45 degrees, far exceeding the maximum safe incline of 17 degrees recommended by the manufacturer. The rescue squad pronounced him dead at the scene [NIOSH 2008].
4. Size of the Vulnerable Population
 The next task in exploring these overlapping vulnerabilities is getting a better idea of the size of the population that shares these characteristics (that is, how many Hispanic immigrants are young workers and how many are employed in small construction firms). According to U.S. Census data, in 2013, the total number of construction workers employed in businesses with fewer than 10 employees was almost 2 million (1,873,475) [U.S. Census Bureau 2014b]. Of the nearly 1.5 million (1,482,495) Hispanic immigrants working in construction, about 40% (551,928) worked in firms with fewer than 10 employees. The proportion is similar for young workers. In 2013, there were over three-quarters of a million (758,613) construction workers aged 24 or younger, of whom nearly a third (221,531) worked in construction firms with fewer than 10 employees.
The next task in exploring these overlapping vulnerabilities is getting a better idea of the size of the population that shares these characteristics (that is, how many Hispanic immigrants are young workers and how many are employed in small construction firms). According to U.S. Census data, in 2013, the total number of construction workers employed in businesses with fewer than 10 employees was almost 2 million (1,873,475) [U.S. Census Bureau 2014b]. Of the nearly 1.5 million (1,482,495) Hispanic immigrants working in construction, about 40% (551,928) worked in firms with fewer than 10 employees. The proportion is similar for young workers. In 2013, there were over three-quarters of a million (758,613) construction workers aged 24 or younger, of whom nearly a third (221,531) worked in construction firms with fewer than 10 employees.
Young Hispanic immigrants are more likely to work for a very small business than are other racial and ethnic groups that make up much of the construction workforce. In 2013, approximately 121,560 foreign-born Hispanics employed in construction were 16 to 24 years of age (8.2% see Table 1), and from 2009 to 2013, just under half of all young Hispanic immigrants in construction worked for a very small business (59,320 for 2013, based on the percentages provided in Tables 1 and 2). There were approximately three times as many foreign-born Hispanic workers as native-born Hispanic construction workers, and a greater proportion of younger foreign-born workers were employed in the smallest construction establishments than were their native-born Hispanic and white, non-Hispanic counterparts.
| Age Group |
2009 | 2011 | 2013 | ||||||
| Hispanic, Foreign- born |
Hispanic, Native |
White non- Hispanic |
Hispanic, Foreign- born |
Hispanic, Native |
White non- Hispanic |
Hispanic, Foreign- born |
Hispanic, Native |
White non- Hispanic |
|
| 16–24 | 10.4% | 13.9% | 10.5% | 8.7% | 14.5% | 10.0% | 8.2% | 20.0% | 11.5% |
| 25–34 | 37.6% | 40.7% | 23.6% | 35.3% | 35.8% | 23.9% | 33.9% | 28.5% | 25.8% |
| 35–44 | 31.9% | 20.1% | 22.7% | 32.2% | 23.0% | 22.3% | 30.5% | 27.7% | 22.2% |
| 45-54 | 15.6% | 18.8% | 26.6% | 18.2% | 16.0% | 25.4% | 19.6% | 15.7% | 21.8% |
| 55-64 | 3.1% | 5.5% | 13.9% | 4.4% | 8.0% | 15.1% | 7.4% | 7.4% | 15.1% |
| 65+ | 1.4% | 0.9% | 2.7% | 1.2% | 2.7% | 3.3% | 0.3% | 0.7% | 3.7% |
| Total | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 100% |
| Weighted number |
1,309,700 | 414,400 | 4,183,300 | 1,307,600 | 472,900 | 4,088,600 | 1,482,500 | 476,400 | 4,307,700 |
| Source: 2010–2014 March Supplement to the Current Population Survey, U.S. Census Bureau. Calculations by CPWR Data Center. Note: Wage and salary workers only. Only odd years are presented to concisely demonstrate 5-year trends. |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Age 16-24 | |||
| Year | Hispanic, Foreign- born |
Hispanic, Native |
White, non- Hispanic |
| 2009 | 44.9% | 34.1% | 32.1% |
| 2010 | 51.5% | 42.7% | 38.4% |
| 2011 | 31.4% | 29.6% | 31.2% |
| 2012 | 41.3% | 33.0% | 42.0% |
| 2013 | 48.8% | 34.0% | 26.7% |
| Average | 43.6% | 34.7% | 34.1% |
| Source: 2010–2014 March Supplement to the Current Population Survey, U.S. Census Bureau. Calculations by CPWR Data Center. Note: Wage and salary workers only. Those without establishment information were excluded. |
|||
|---|---|---|---|
Additionally, according to estimates based on the National Health Interview Survey [CDC 2013] (see Table 3), approximately two-thirds of Hispanic construction workers in the United States in 2013 were not citizens, a factor that has been identified as a possible contributor to occupational health disparities among immigrants [Schenker 2010; Flynn 2010]. These survey data, shown in Table 3, also indicate nearly one quarter (23.5%) of all U.S. Hispanic construction workers have been on the job for less than a year, and nearly three quarters (70.4%) have been on the job for less than 5 years. One potential occupational health barrier identified by this survey is the high proportion (81.9%) of Hispanic construction workers who report they receive no paid sick leave. This proportion is higher than among the overall construction sample (75.7% with no paid sick leave) and much higher than among the overall working population in the survey (43.4%), which is noteworthy because previous research suggests paid sick leave may help businesses reduce the incidence of nonfatal occupational injuries [Asfaw et al. 2012]. The data presented in Table 3 also support the conclusions from the Current Population Survey data that the majority of Hispanic construction workers in the United States are foreign born, and a significant proportion work for a small business establishment with fewer than 10 employees.
| Hispanic construction workers | |||
| Employment characteristics | |||
| Population estimate | n | % | |
| TOTAL | 2,148,307 | 330 | 100.0 |
| Age/years | |||
| 18–19 | 28,208 | 3 | 1.3% |
| 20–24 | 179,209 | 22 | 8.3% |
| 25–34 | 721,110 | 112 | 33.6% |
| 35–44 | 665,675 | 105 | 31.0% |
| 45–54 | 344,409 | 54 | 16.0% |
| 55–64 | 175,745 | 27 | 8.2% |
| 65+ | 33,951 | 7 | 1.6% |
| Citizenship status | |||
| Yes, US Citzen | 747,988 | 109 | 34.9% |
| Not a US Citzen | 1,393,693 | 220 | 65.1% |
| Born in the U.S. | |||
| Yes, Born in U.S. | 383,573 | 56 | 17.9% |
| Foreign-Born | 1,764,734 | 274 | 82.1% |
| Number of employees at work | |||
| 1–9 | 1,092,776 | 175 | 53.9% |
| 10–24 | 380,474 | 56 | 18.8% |
| 25–49 | 178,701 | 27 | 8.8% |
| 50–99 | 185,038 | 27 | 9.1% |
| 100+ | 192,140 | 29 | 9.5% |
| Number of years on the job | |||
| Less than 1 year | 439,116 | 68 | 23.5% |
| 1–5 | 876,271 | 133 | 46.9% |
| 6–10 | 223,055 | 36 | 12.0% |
| 11–15 | 186,655 | 28 | 10.0% |
| 15 years or more | 141,345 | 21 | 7.6% |
| Paid sick leave at current job | |||
| Yes | 378,878 | 54 | 18.1% |
| No | 1,719,891 | 268 | 81.9% |
The census data provide an overall sense of the numbers of individuals who fall into each of the overlapping vulnerable populations of young Hispanic immigrants working in small businesses, and the National Health InterTable view Survey data provide some additional details about these groups. The Mexican Ministry of Governance conducts a regular census of immigrants returning to Mexico (Border Survey of Mexican Migration, or EMIF Norte, Consejo Nacional de Poblacion [CONAPO 2010]), and it recently included questions about OSH. This data source provides some evidence that the occupational health experiences of Hispanic immigrants who have worked for small businesses in the United States place them at elevated risk for injury and illness.
Among immigrants returning to Mexico from January to March 2010 (n = 5,458), approximately 75% of respondents worked for a business with 50 or fewer employees (see Figure 1). This percentage is nearly the inverse of the proportion (28%) of U.S. workers that were employed in an establishment with fewer than 50 employees in 2007 [U.S. Census Bureau 2011]. This finding alone is cause for greater attention to the issue of overlapping vulnerabilities.
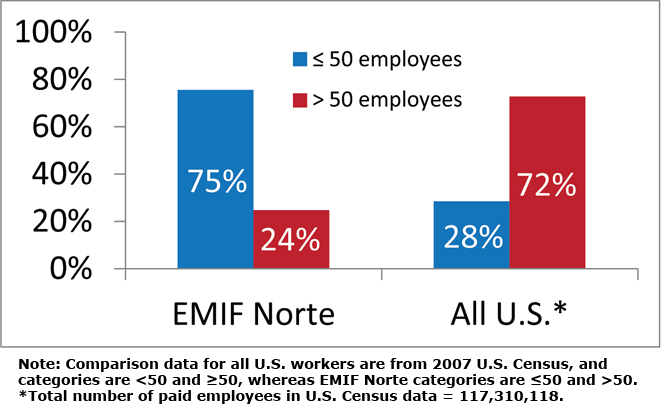
Figure 1. Percent of workforce employed by smaller or larger businesses.
Persons who worked for smaller establishments were less likely to get training (28% of respondents in workplaces with 50 or fewer employees received training, compared with 39% in workplaces with more than 50 employees). Additionally, those who worked for smaller establishments were less likely to sign a contract with their employer and were less likely to have benefits.
The median age among immigrants returning to Mexico who worked while they were in the United States was 38 years. This is lower than the median age of 42 years in the U.S. workforce [BLS 2013]. Although this finding does not necessarily mean there is a greater proportion of young workers among immigrants working in the United States than among native-born workers, these data mirror a similar pattern in data for Hispanic-origin workers in the United States versus the overall U.S. workforce [BLS 2013].
On the basis of these data, one can conclude it is likely that Hispanic immigrants working in the U.S. face greater OSH challenges than native-born workers, not only because of the unique barriers they encounter as immigrants but also because of the lack of OSH resources available in smaller businesses, where the majority of Hispanic immigrants are employed. However, these data are rather limited in that they include only a very small number of the ~19 million Hispanic immigrants living in the United States and only immigrants returning to Mexico.
5. Conceptualizing Overlapping Vulnerabilities and Their Interaction
 The third step in looking at overlapping vulnerabilities is understanding how they interact with one another, and the degree to which they present unique barriers to reducing these disparities. As described in the preceding sections, a growing body of literature addresses occupational health disparities in the construction industry and explores how particular groups of workers are at an increased risk for occupational injury or illness. These articles often address the unique risks, barriers to safety, and possible interventions for groups such as young workers, immigrants, and small business employees and owners. A scan of the literature published since 1995 was conducted1. This scan was not an exhaustive review, but provided a general idea of the degree to which the overlap of the identified vulnerabilities is addressed in the literature.
The third step in looking at overlapping vulnerabilities is understanding how they interact with one another, and the degree to which they present unique barriers to reducing these disparities. As described in the preceding sections, a growing body of literature addresses occupational health disparities in the construction industry and explores how particular groups of workers are at an increased risk for occupational injury or illness. These articles often address the unique risks, barriers to safety, and possible interventions for groups such as young workers, immigrants, and small business employees and owners. A scan of the literature published since 1995 was conducted1. This scan was not an exhaustive review, but provided a general idea of the degree to which the overlap of the identified vulnerabilities is addressed in the literature.
Of the 48 papers reviewed, only 17 addressed at least two of the three vulnerabilities central to this report (see Table 4). Only two articles were found that addressed all three characteristics (young workers, Hispanic immigrants, and small business employees) [Dong et al. 2013; Dong et al. 2014]. In general, the researchers found that each of the three vulnerabilities placed workers at higher risk for negative occupational health outcomes. However, the majority of the articles addressed each of the vulnerabilities independently and did not examine how the risk may change for an individual who belongs to more than one of these groups.
| Study (Number of subjects) | Study type | Size of firm |
Age of employee |
Native vs foreign born |
| Forst et al. 2013 (446) | Intervention | - | C | C |
| Sokas et al. 2009 (92) | Intervention | - | C | R |
| Flynn and Sampson 2012 (40) | Risk Factor | C | R | - |
| Arcury et al. 2014 (87) | Risk Factor | - | R | R |
| Nissen 2008 (283) | Risk Factor | - | R | R |
| O’Connor et al. 2005 (50) | Risk Factor | - | R | R |
| Grzywacz et al. 2012 (108) | Risk Factor | - | R | R |
| Holte et al. 2014 (673) | Risk Factor | R | R | - |
| Pedersen et al. 2012 (183,738) | Risk Factor | R | R | - |
| Darragh et al. 2004 (97 frms) | Intervention | R | R | - |
| Suruda et al. 2003 (326) | Risk Factor | R | R | - |
| Polivka 1996 (3,422,000)* | Risk Factor | - | R | - |
| Buchanan et al. 2005 (21)* | Risk Factor | - | R | R |
| Contreras and Buchanan 2012 (42)* | Intervention | - | R | R |
| Steege et al. 2014 (26,996) | Risk Factor | - | R | R |
| Papers that address more than two vulnerabilites | ||||
| Dong et al. 2014 (2,986) | Risk Factor | R | R | R |
| Dong et al. 2013 (8,123) | Risk Factor | R | R | R |
| C = collected during the study but not used for reporting or analysis. R = reported and/or used in analysis, to some degree. *Also addresses temporary vs. permanent employment status. |
||||
|---|---|---|---|---|
Two articles addressed the overlap or interrelatedness of two of the vulnerabilities. Suruda et al. [2003] showed how fatal injuries for teenage construction workers tended to concentrate in small businesses, more so than for adults. O’Connor et al. [2005] explored the adequacy of safety and health training for young Hispanic immigrant construction workers, because being both young workers and immigrants put them at risk. They found that a quarter of the Hispanic teens working in construction received no safety training and approximately a quarter received less than one hour of training. Given the lack of research that focuses on overlapping vulnerabilities across all industries, generally, and in the construction sector, specifically, more work needs to be done to document how these different vulnerabilities may overlap and interact.
A critical next step for improving OSH outcomes among vulnerable populations is to build on the work that addresses multiple vulnerabilities when developing safety programs and interventions. Each of these vulnerable populations brings unique barriers that are not shared across groups. Figure 2 illustrates a way to visualize areas of overlap for specific vulnerable groups. Consider that Hispanic immigrants may have language barriers, young workers may not feel comfortable voicing safety concerns, and small business employees may not have access to up-to-date safety training. Although each of these barriers is associated with a particular vulnerable group, many workers experience more than one of these barriers because they belong to multiple vulnerable groups. For example, young Hispanic immigrant workers (area 2 in Figure 2) may be at even greater risk of occupational injury or illness because they experience both language difficulties and hesitation to voice safety concerns on account of power differentials they associate with age differences and fear of reprisals (such as being fired or having their documentation status questioned).
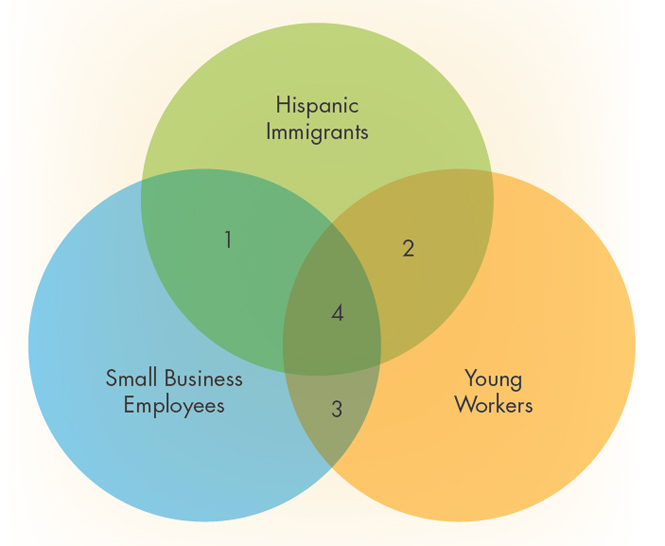
Figure 2. Overlap of OSH vulnerabilities.
In another example, a Hispanic immigrant working in a larger organization may feel unsafe performing a particular task such as working from a ladder. As an immigrant, the worker may be unable to speak to the supervisor because of a language barrier. However, because he or she works in a larger organization, there may be a safety professional on the job, supervisory support for stopping work to address a safety concern, bilingual employees who can coach the worker through the task, training available to safely perform the work, and/or safety equipment available to help perform the task more safely. Any or all of these forms of assistance may help the worker overcome or neutralize the language barrier. A Hispanic immigrant in a smaller business may also be reluctant to speak to the supervisor, but the language barrier may be more insurmountable without the supports that are available at the larger organization (area 1 in Figure 2).
Other limitations arise in addressing only one of multiple vulnerabilities for a given population of workers, rather than assessing how multiple vulnerabilities overlap and interact (area 4 in Figure 2). For example, numerous organizations have developed Spanish-language OSH training materials. Indeed, some of these materials have been specifically tailored not only to the language needs of Hispanic immigrants, but also to the cultural context in which these workers operate [Scruggs and Arroyo 2014]. However, these training materials have not necessarily been developed to address the concerns of young workers or with consideration for their use by small employers. Thus, many in the intended audience (areas 1, 2, and 4 in Figure 2) may not benefit from the intervention effort because barriers related to only one aspect of their OSH vulnerabilities (that is, being an immigrant) were being considered during intervention development. Such training intervention efforts might be enhanced by considering the unique barriers younger workers encounter and what is feasible for smaller contractors to implement, or delivery mechanisms that take into account how they might see value in supporting OSH training for the Hispanic immigrant workforce from which they draw employees.
 In conclusion, an additive or compound effect of multiple vulnerability factors may influence OSH outcomes for vulnerable individuals. Although the specific mechanisms and quantitative effects of these interactions are beyond the scope of this report and require additional research, OSH practitioners can significantly improve their OSH outreach efforts by considering the multiple vulnerable groups their target audiences may include.
In conclusion, an additive or compound effect of multiple vulnerability factors may influence OSH outcomes for vulnerable individuals. Although the specific mechanisms and quantitative effects of these interactions are beyond the scope of this report and require additional research, OSH practitioners can significantly improve their OSH outreach efforts by considering the multiple vulnerable groups their target audiences may include.
6. Interventions that Address OSH Vulnerabilities
 Numerous efforts have shown promise in addressing the unique needs of vulnerable workers. Interventions, such as those described below, could be expanded to address multiple vulnerabilities. These examples certainly do not cover the entire range of positive efforts by various organizations to address vulnerable worker groups, but they do provide several elements of interventions that OSH professionals may consider for more effectively assisting vulnerable worker and employer groups with OSH.
Numerous efforts have shown promise in addressing the unique needs of vulnerable workers. Interventions, such as those described below, could be expanded to address multiple vulnerabilities. These examples certainly do not cover the entire range of positive efforts by various organizations to address vulnerable worker groups, but they do provide several elements of interventions that OSH professionals may consider for more effectively assisting vulnerable worker and employer groups with OSH.
For example, on the larger strategic level, NIOSH has developed a binational partnership with the Mexican government to identify and address occupational health inequities among immigrant workers [Flynn et al. 2013]. This collaboration focuses on three key areas: research and surveillance, outreach, and building institutional capacity. With assistance from NIOSH, the Mexican government institutionalized OSH as a priority topic for health promotion through the Ventanillas de Salud, the country’s public health outreach program in the United States. NIOSH is currently assisting with efforts to link health promotion, legal services, and research activities to improve the OSH of Mexicans living in the United States [O’Connor et al. 2014]. This partnership couples NIOSH technical expertise with existing Mexican government systems. Although this has been a very successful partnership, it is important to note that Hispanic immigrants come from many countries and the appropriate institutions for reaching workers may vary from one national group to the next.
In another example, New Labor, a membership- based worker center in New Jersey, implemented a program to teach immigrant day laborers to serve as peer safety leaders. The program trained the laborers to recognize safety and health hazards, to communicate effectively with coworkers and supervisors, and to facilitate tailored OSHA 10-hour training. By 2014, more than 500 workers in New Jersey and New York received OSHA 10-hour cards through this program [Scruggs and Arroyo 2014].
 NIOSH developed a model for OSH intervention diffusion to small businesses based on existing research on using intermediary organizations as delivery channels. Examples of intermediaries include suppliers of goods and services to small businesses, such as trade associations, insurers, chambers of commerce, building supply stores, and unions. These organizations provide infrastructure that facilitates intervention delivery between initiating public health/safety agencies and the small businesses as a means of overcoming the resource scarcity issue [Hasle and Limborg 2006; Hasle et al. 2012; Olsen et al. 2012]. Intermediaries can also provide an infrastructure for evaluating intervention efforts. This model can be referred to as an initiator–intermediary– small business diffusion model [Cunningham and Sinclair 2015; Sinclair et al. 2013]. This model has been applied successfully with several intermediary organizations in multiple targeted areas, including trenching in construction [Cunningham and Sinclair 2015]. Results of these applications of the model indicated that intermediary organizations were highly attuned to providing smaller businesses with what they want, including OSH services. This recommendation has been echoed specifically to address the potential role of intermediaries in reaching contractors who employ Hispanic workers [Scruggs and Arroyo 2014].
NIOSH developed a model for OSH intervention diffusion to small businesses based on existing research on using intermediary organizations as delivery channels. Examples of intermediaries include suppliers of goods and services to small businesses, such as trade associations, insurers, chambers of commerce, building supply stores, and unions. These organizations provide infrastructure that facilitates intervention delivery between initiating public health/safety agencies and the small businesses as a means of overcoming the resource scarcity issue [Hasle and Limborg 2006; Hasle et al. 2012; Olsen et al. 2012]. Intermediaries can also provide an infrastructure for evaluating intervention efforts. This model can be referred to as an initiator–intermediary– small business diffusion model [Cunningham and Sinclair 2015; Sinclair et al. 2013]. This model has been applied successfully with several intermediary organizations in multiple targeted areas, including trenching in construction [Cunningham and Sinclair 2015]. Results of these applications of the model indicated that intermediary organizations were highly attuned to providing smaller businesses with what they want, including OSH services. This recommendation has been echoed specifically to address the potential role of intermediaries in reaching contractors who employ Hispanic workers [Scruggs and Arroyo 2014].
 In another example of a promising strategy to address occupational health disparities among Hispanic immigrants working in small construction businesses, researchers in San Francisco and Philadelphia assessed perceptions of barriers to fall prevention among both workers and contractors. Key lessons learned centered around contractors as being the most important target audiences, the need for clear, strong incentives for contractors to provide rather than ignore fall protection measures, and that fall protection training for Latino immigrant workers should include content on immigrant and worker rights, and addressing barriers. On the basis of their findings, they identified contractor associations, unions, worker centers, and other partners they could leverage to influence contractors to promote safer fall-prevention practices. These intermediary organizations offered OSHA 10-hour training to workers and employers, and each of the target audiences was incentivized to participate: workers could pursue employment opportunities, small businesses were able to find OSHA-10-hour-certified workers, and trade associations were able to offer a benefit to their members [Scruggs and Arroyo 2014].
In another example of a promising strategy to address occupational health disparities among Hispanic immigrants working in small construction businesses, researchers in San Francisco and Philadelphia assessed perceptions of barriers to fall prevention among both workers and contractors. Key lessons learned centered around contractors as being the most important target audiences, the need for clear, strong incentives for contractors to provide rather than ignore fall protection measures, and that fall protection training for Latino immigrant workers should include content on immigrant and worker rights, and addressing barriers. On the basis of their findings, they identified contractor associations, unions, worker centers, and other partners they could leverage to influence contractors to promote safer fall-prevention practices. These intermediary organizations offered OSHA 10-hour training to workers and employers, and each of the target audiences was incentivized to participate: workers could pursue employment opportunities, small businesses were able to find OSHA-10-hour-certified workers, and trade associations were able to offer a benefit to their members [Scruggs and Arroyo 2014].
In an effort targeting both employers with fewer than 50 employees and Spanish-speaking employers, the Labor and Occupational Health Program [LOHP 2015] at the University of California, Berkeley, has developed a model training program that teaches small business owners and managers to develop and implement their own injury and illness prevention programs (IIPPs). The model program includes a half-day interactive training session and a guide for writing an IIPP. The sessions are conducted by trainers from LOHP and Cal/OSHA Consultation Service. Although evaluation data have not yet been published, this effort is a clear example of assisting employers to deliver effective IIPPs to workers who are vulnerable not only because they are in small businesses, but also possibly because they are immigrants. The LOHP also found California’s State Compensation Insurance Fund to be a valuable intermediary and partner in bringing people to the training.
 In interventions focused on young workers in construction, much of the effort is on educational settings. A recent report on integrating OSH training into career technical education in construction noted that teaching the OSHA-10 (usually providing students with OSHA-10 cards) is almost universal at the community college level and is growing at the high school level [Bush and Andrews 2013]. The same report also notes that when educators rely on the OSHA-10 as the primary classroom content, their students may not be learning all of the basic foundational and leadership OSH skills they will need. To address such concerns, NIOSH and its partners have developed Youth@ Work—Talking Safety [NIOSH 2014], a free curriculum that teaches foundational workplace safety and health skills and knowledge, known as the NIOSH 8 Core Competencies. The curriculum covers basic infor¬mation relevant to any occupation at any stage of work life. The Core Competencies include the ability to:
In interventions focused on young workers in construction, much of the effort is on educational settings. A recent report on integrating OSH training into career technical education in construction noted that teaching the OSHA-10 (usually providing students with OSHA-10 cards) is almost universal at the community college level and is growing at the high school level [Bush and Andrews 2013]. The same report also notes that when educators rely on the OSHA-10 as the primary classroom content, their students may not be learning all of the basic foundational and leadership OSH skills they will need. To address such concerns, NIOSH and its partners have developed Youth@ Work—Talking Safety [NIOSH 2014], a free curriculum that teaches foundational workplace safety and health skills and knowledge, known as the NIOSH 8 Core Competencies. The curriculum covers basic infor¬mation relevant to any occupation at any stage of work life. The Core Competencies include the ability to:
- Recognize that work has both benefits and risks, and that all workers can be injured, become sick, or even be killed on the job
- Recognize that work-related injuries and illnesses are predictable and can be prevented
- Identify hazards at work and predict how workers can be injured or made sick
- Recognize how to prevent injury and illness
- Identify emergencies at work and decide on the best ways to address them
- Recognize employer and worker rights and responsibilities
- Find resources that help keep workers safe and healthy on the job
- Demonstrate how to communicate effectively with others on the job when feeling unsafe.
 Integrating foundational workplace safety and health skills as missing life skills into curricula may be one way to ensure that every individual, before entering the workforce, has the basic workplace knowledge and skills necessary to engage in safe and healthy work. Currently, demonstration projects are under way in five states (California, Florida, New York, Oklahoma, and Oregon) to find ways to integrate the competencies delivered through Talking Safety in school- and community-based programs, youth development organizations, professional organizations, and temporary employment agencies.
Integrating foundational workplace safety and health skills as missing life skills into curricula may be one way to ensure that every individual, before entering the workforce, has the basic workplace knowledge and skills necessary to engage in safe and healthy work. Currently, demonstration projects are under way in five states (California, Florida, New York, Oklahoma, and Oregon) to find ways to integrate the competencies delivered through Talking Safety in school- and community-based programs, youth development organizations, professional organizations, and temporary employment agencies.
Finally, it is also worth noting that there has been considerable effort toward teaching both employers and employees in the construction industry how to develop a stronger safety culture and safety climate within their organizations and on job sites. Safety culture reflects the organization’s core values and assumptions about safety (espoused, a fixed state, qualitative), while safety climate refers to the shared perceptions about safety among a homogeneous group on site at a given point in time (enacted, variable, quantitative) [Hecker and Goldenhar 2013]. One example of guidance in developing a stronger safety culture in construction is a set of worksheets designed by CPWR to help managers, safety professionals, and hourly craft workers learn about some of the important leading indicators of safety climate as well as ideas for strengthening them [CPWR 2014]. If safety culture among smaller construction firms can be improved, it will help to create an atmosphere where vulnerable workers may be encouraged to speak up and employers are able to communicate more effectively about OSH issues with vulnerable workers.
7. How OSH Interventions May Address Multiple Vulnerabilities
 In light of the examples of interventions provided, several important points should be considered for addressing multiple vulnerabilities. Developing effective interventions requires an understanding of both the unique barriers and assets these groups have. For OSH professionals to be able to more effectively assist workers with multiple vulnerabilities, more work needs to be done in three domains: researching overlapping vulnerabilities, developing and refining interventions, and building sustainable efforts.
In light of the examples of interventions provided, several important points should be considered for addressing multiple vulnerabilities. Developing effective interventions requires an understanding of both the unique barriers and assets these groups have. For OSH professionals to be able to more effectively assist workers with multiple vulnerabilities, more work needs to be done in three domains: researching overlapping vulnerabilities, developing and refining interventions, and building sustainable efforts.
1. Research is needed to understand how different vulnerabilities may overlap and interact with one another in the lived experience of workers. These research needs could be met with the following actions:
- Examining existing data sets to identify groups of workers belonging to more than one vulnerable population and developing methods for collecting data on multiple risk factors
- Adding data fields to existing data-collection efforts related to other key vulnerable populations (for example, when surveying worker populations, gather data on business size, age, years in country, place of birth, work arrangement, etc.)
- Expanding efforts that focus on one vulnerability to consider the potential overlap with other vulnerabilities (such as immigration, age, size of employer, and work arrangement) as more than just alternate explanations of effects or confounding factors to control for.
2. Interventions for a particular group should consider factors such as place of birth, business size, age, and work arrangement to ensure that materials are tailored to address barriers for all relevant vulnerabilities that workers face. Consider intervention elements such as these:
- Culturally tailoring safety certifications and training programs and delivering these trainings through resource-appropriate channels. Vulnerable workers would likely benefit from gaining not only basic OSH skills, such as the ability to identify hazards and understand how they can be controlled, but also leadership skills such as being able to problem-solve and speak up in the workplace.
- Creating interest in safety certifications and training programs as a competitive advantage for workers from vulnerable populations while also creating demand for these credentials among employers. Safety certifications may help to empower vulnerable workers if there is a demand for them among desirable employers. Whereas many larger employers may require particular certifications as a condition of employment, smaller employers may need to be convinced of the value that a prospective employee’s certification or training can add to their business. The business value of employee certification is likely best communicated to employers by the intermediaries within their communities, such as trade associations, insurers, and chambers of commerce.
- Increasing awareness among employers of the increased risks of occupational injury and illness among the vulnerable populations they employ. Many employers are likely already aware of specific challenges such as language barriers or lack of access to training, but they may benefit from additional information about the risks associated with each vulnerability factor that may affect their workforce, as well as training on how to effectively communicate safety information.
- Assisting small employers with basic workplace safety and health activities. Small employers need assistance to implement activities such as hazard recognition and control and writing safety plans in a manner that is both culturally and resource-appropriate for their workplaces.
3. Diffusion of tailored interventions will be most effective by working with the institutions and organizations that already serve these communities. OSH professionals often do not have longstanding institutional relationships with key organizations in these communities, nor the institutional capacity and cultural competence to work effectively with these groups. Likewise, the intervention models that OSH organizations have developed with their partners may not be appropriate for use with these organizations. Effective and sustainable intervention efforts should include these factors:
- Understanding how professionals and institutions working within each of the relevant communities of vulnerable workers can work together to address areas of overlapping vulnerabilities. By partnering, professionals and organizations that were working with separate target groups can expand their networks and create new client or membership opportunities.
- Using established intervention models, such as the initiator–intermediary–small business diffusion model described in this report, to reach vulnerable populations. Such models place responsibility on both initiators and intermediaries to develop and market interventions that will be valued.
- Developing longstanding, institutional relationships with key organizations who work within communities of vulnerable workers and employers. OSH professionals and organizations will need to network and interact to identify and build relationships within each of these communities. Utilizing webpages and social media campaigns can support intervention efforts, but a concerted effort to build relationships among OSH professionals and key community organizations will likely provide a greater and more sustainable impact.
- Working to integrate OSH into current activities and efforts that new partner organizations are already doing. These new partner organizations need not necessarily be work-focused (such as faith-based organizations or hometown associations for a particular nationality), but they should be a trusted source of information and active within the community. Adding OSH elements to their ongoing activities that may not have been specifically OSH-focused increases the chances that interventions will be tailored to the needs of the community and the institutional capacity of the partner organization. Adding an OSH component to ongoing activities also limits the burden of the intervention on the partner and allows OSH professionals to benefit from their existing infrastructure. This often limits the scope of the intervention and requires some flexibility. However, it is often a more sustainable model and can facilitate the development of long-term institutional relationships.
- Conducting data-driven evaluations of intervention efforts to demonstrate their effectiveness. Previous interventions have included such evaluations to varying degrees. OSH professionals and community organizations will be better able to assess and improve the impact of their efforts among vulnerable populations if effective measures are in place to evaluate their efforts. The initiating public health/safety organizations can also assist with evaluation.
 The American Society of Safety Engineers (ASSE) and NIOSH are the initiators of an effort to reach workers who experience overlapping OSH vulnerabilities in small construction businesses with an intervention to improve OSH. This is a diverse and particularly vulnerable target audience that is not likely to be reached by a single communication effort directly from either ASSE or NIOSH. On the basis of the considerations offered in this report for effectively intervening to improve OSH among workers with multiple, overlapping vulnerabilities, the specific content and delivery of such an intervention will depend on the engagement and input of key intermediaries. Thus, intermediaries and OSH professionals who are in direct contact with employers of workers experiencing overlapping vulnerabilities should join this effort. They will likely find value in offering OSH assistance to vulnerable workers and employers, not only in terms of protecting workers, promoting socially responsible practices, and enhancing public perceptions and relations, but also in the opportunities for new business relationships, such as in training new audiences, creating an expanded referral network, bringing on new clients, and adding value to existing memberships or client relationships.
The American Society of Safety Engineers (ASSE) and NIOSH are the initiators of an effort to reach workers who experience overlapping OSH vulnerabilities in small construction businesses with an intervention to improve OSH. This is a diverse and particularly vulnerable target audience that is not likely to be reached by a single communication effort directly from either ASSE or NIOSH. On the basis of the considerations offered in this report for effectively intervening to improve OSH among workers with multiple, overlapping vulnerabilities, the specific content and delivery of such an intervention will depend on the engagement and input of key intermediaries. Thus, intermediaries and OSH professionals who are in direct contact with employers of workers experiencing overlapping vulnerabilities should join this effort. They will likely find value in offering OSH assistance to vulnerable workers and employers, not only in terms of protecting workers, promoting socially responsible practices, and enhancing public perceptions and relations, but also in the opportunities for new business relationships, such as in training new audiences, creating an expanded referral network, bringing on new clients, and adding value to existing memberships or client relationships.
Examples of Potential Barriers to Improving OSH Outcomes
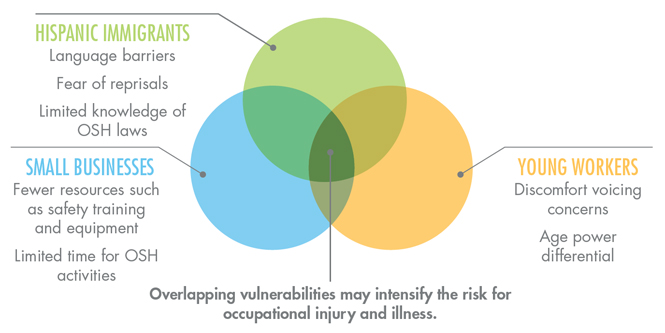
Join the Conversation
 The risk to these workers cannot be impacted by a single communication effort from ASSE and NIOSH. Interventions will depend on the engagement and input of OSH professionals who are in direct contact with employers of workers experiencing overlapping vulnerabilities.
The risk to these workers cannot be impacted by a single communication effort from ASSE and NIOSH. Interventions will depend on the engagement and input of OSH professionals who are in direct contact with employers of workers experiencing overlapping vulnerabilities.
Read more at www.asse.org/workersatriskESSA
8. Endnotes and References
Endnotes
1The literature scan in this report was conducted with Google Scholar in December 2014 (key words: Latino construction workers, small business construction workers, subcontractor construction safety, contracted and subcontracted employee construction safety, young construction workers) to search for evidence relevant to overlapping vulnerabilities among young workers, Hispanic workers, and small business employees in the construction industry. Results from the first 15 search pages were examined, and relevant publications were included in the scan. Additionally, articles from published literature reviews were examined [Scruggs and Arroyo 2014; van der Molen et al. 2012; Chapman 2013], as well as relevant articles known to the authors. The scan identified and evaluated forty-eight (48) studies: twenty-one (21) about Hispanic workers or Hispanic construction workers, eleven (11) studies of people working for small business, and sixteen (16) studies of younger workers.
2This scan of the literature focused on Hispanic immigrant status, small business, and young workers. However, there are a number of factors that could be explored. For example, temporary work status is another factor that warrants further research, on its own and in interaction with other vulnerabilities, such as immigrant or youth status. Not only are temporary workers often exposed to hazardous working conditions, but they also tend to have less job experience and safety training, a combination that can increase their risk of occupational injury [Benavides et al. 2006; Walter et al. 2002]. Temporary employment is very common in the construction industry, which has been found to have the highest prevalence rate for nonstandard work, at 44% [Alterman et al. 2013]. About 12% of construction companies use day laborers, 22% of companies have no full-time employees, and 8% hire workers through temporary agencies [CPWR 2013]. Using data from workers’ compensation claims in Washington State, Smith and colleagues [2010] found that temporary workers had higher injury rates than did permanent employees for all injury types in the construction industry. Temporary workers who experience occupational injuries may not report their injuries due to a lack of knowledge about occupational health rights or a fear of jeopardizing future employment opportunities [Nicholson et al. 2008]. Further research is needed to explore this disparity and better inform intervention efforts.
References
Alterman T, Luckhaupt SE, Dahlhamer JM, Ward BW, Calvert GM [2013]. Prevalence rates of work organization characteristics among workers in the U.S.: data from the 2010 National Health Interview Survey. Am J Ind Med 56:647–659.
Arcury TA, Summers P, Carrillo L, Grzywacz JG, Quandt SA, Mills TH [2014]. Occupational safety beliefs among Latino residential roofing workers. Am J Ind Med 57(6):718–725.
Asfaw A, Pana-Cryan R, Rosa R [2012]. Paid sick leave and nonfatal occupational injuries. Am J Publ Health 102(9):e59–e64.
Baron SL, Steege AL, Marsh SM, Chaumont Menéndez C, Myers JR [2013]. Nonfatal work-related injuries and illnesses: United States, 2010. Morbid Mortal Wkly Rep 26(3):35–40.
Belman D, Levine D [2004]. Size, skill, and sorting. Labour 18:515–561.
Benavides FG, Benach J, Muntaner C, Delclos GL, Catat N, Amable M [2006]. Associations between temporary employment and occupational injury: what are the mechanisms? Occup Environ Med 63:416–421.
BLS [2005]. Work activity of high school students: data from the National Longitudinal Survey of Youth 1997, http://www.bls.gov/nls/nlsy97r6.pdf.
BLS [2006]. Occupational outlook handbook, 2006–2007, http://www.bls.gov/oco/.
BLS [2013]. Median age of the labor force, by sex, race and ethnicity, http://www.bls.gov/emp/ep_table_306.htm.
BLS [2014a]. Census of fatal occupational injuries charts, 1992–2013. Retrieved from http://www.bls.gov/iif/oshwc/cfoi/cfch0012.pdf
BLS [2014b]. Employed persons by detailed industry and age, http://www.bls.gov/cps/cpsaat18b.pdf.
BLS [2014c]. Nonfatal occupational injury and illnesses requiring days away from work, 2013, http://www.bls.gov/news.release/pdf/osh2.pdf.
BLS [2014d]. Fatal occupational injuries by selected worker characteristics and selected event or exposure, 2013, http://www.bls.gov/news.release/cfoi.t04.htm.
BLS [2014e]. National census of fatal occupational injuries in 2013 (preliminary results), http://www.bls.gov/news.release/pdf/cfoi.pdf.
Breslin FC, Day D, Tompa E, Irvin E, Bhattacharyya S, Clarke J, Wang A [2007]. Non-agricultural work injuries among youth: a systematic review. Am J Prevent Med 32(2):151–162.
Buchanan SN, Nickels L, Morello J [2005]. Occupational health among Chicago day laborers: an exploratory study. Arch Environ Occup Health 60(5):276–280.
Buckley JP, Sestito JP, Hunting KL [2008]. Fatalities in the landscape and horticultural services industry, 1992–2001. Am J Ind Med 51:701–713.
Bush D, Andrews K [2013]. Integrating occupational safety and health training into career technical education in construction: formative research findings, http://www.cpwr.com/sites/default/files/publications/Integrating_ SandH_in_CTE_Training_Bush_2013.pdf.
Castillo D, Lewko J [2013]. Youth employment and the health and safety issues of young workers in the U.S. and Canada: an overview. In: Runyan CW, et al., eds. Health and safety of young workers: proceedings of a U.S. and Canadian series of symposia. Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; and Ontario Neurotrauma Foundation.
CDC [2004]. Occupational fatalities during trenching and excavation work: United States, 1992–2001. MMWR Morbid Mortal Wkly Rep 53(15):311–314.
CDC [2008]. Work-related injury deaths among Hispanics: United States, 1992–2006. MMWR Morbid Mortal Wkly Rep 57(22):596–600.
CDC [2010]. Occupational injuries and deaths among younger workers: United States, 1998–2007. MMWR Morbid Mortal Wkly Rep 59(15):449–455.
CDC [2011]. Rationale for regular reporting on health disparities and inequalities: United States. MMWR Morbid Mortal Wkly Rep 60(1):3–10.
CDC [2013]. National Health Interview Survey, http://www.cdc.gov/nchs/nhis.htm.
Chapman LJ [2013]. Literature review for better translation of research to practice in residential construction, http://www.cpwr.com/sites/default/files/publications/residential_construction_r2p_literature_review_chapman.pdf.
Cheadle A, Franklin G, Wolfhagen C, Savarino J, Liu PY, Salley C et al. [1994]. Factors influencing the duration of work-related disability: a population-based study of Washington state workers’ compensation. Am J Publ Health 84(2):190–196.
Choi E, Spletzer J [2012]. The declining average size of establishments: evidence and explanations. Monthly Labor Rev 50–65.
CONAPO [2010]. Encuesta sobre migración en la frontera norte de México (EMIF Norte), http://www.conapo.gob.mx/index.php?option=com_contentview=article&id=94&Itemid=252.
Congressional Budget Office [2005]. The role of immigrants in the U.S. labor market. Washington, DC: U.S. Government Printing Office.
Connell J [1993]. Kitanai, kitsui and kiken: the rise of labour migration to Japan. Sidney: University of Sydney, Economic and Regional Restructuring Research Unit.
Contreras E, Buchanan S [2012]. Piloting a personal protection equipment distribution program among Chicago day laborers. Am J Ind Med 55(2):159–166.
CPWR [2013]. The construction chart book: the US construction industry and its workers. 5th Ed, http://www.cpwr.com/publications/construction-chart-book.
CPWR [2014]. Strengthening jobsite safety climate by using and improving leading indicators, http://www.cpwr.com/safety-culture/strengthening-jobsite-safety-climate.
Cunningham TR, Sinclair R [2015]. Application of a model for delivering occupational safety and health to smaller businesses: case studies from the U.S. Safety Sci 71:213–225.
Cunningham TR, Sinclair R, Schulte P [2014]. Better understanding the small business construct to advance research on delivering workplace health and safety. Intl J Small Enterprise Res 21(2):148–160.
Cutter S, Boruff B J, Shirley WL [2005]. Social vulnerability to environmental hazards. Soc Sci Q. 84(2); 242–261.
Darragh AR, Stallones L, Bigelow PL, Keefe TJ [2004]. Effectiveness of the HomeSafe Pilot Program in reducing injury rates among residential construction workers, 1994–1998. Am J Ind Med 45(2):210–217.
Dennis WJ, ed. [2002]. National small business poll: workplace safety. Washington, DC: National Federation of Independent Businesses.
Dong XS, Choi SD, Borchardt JG, Wang X, Largay JA [2013]. Fatal falls from roofs among US construction workers. J Safety Res 44:17–24.
Dong XS, Fujimoto A, Ringen K, Stafford E, Platner JW, Gittleman JL, Wang X [2011]. Injury underreporting among small establishments in the construction industry. Am J Ind Med 54(5): 339–349.
Dong XS, Wang X, Daw C [2010]. Fatal and nonfatal injuries among Hispanic construction workers. CPWR Data Brief 2(2):1–19.
Dong XS, Wang X, Largay JA, Platner JW, Stafford E, Cain CT, Choi SD [2014]. Fatal falls in the US residential construction industry. Am J Ind Med 57(9):992–1000.
Eakin JM, MacEachen E [1998]. Health and the social relations of work: a study of the health-related experiences of employees in small businesses. Sociol Health Illness 20:896–914.
Eakin JM, Champoux D, MacEachen E [2010]. Health and safety in small workplaces: refocusing upstream. Can J Public Health 101(Suppl 1):529–533.
Fabiano B, Curro F, Pastorino R [2004]. A study of the relationship between occupational injuries and firm size and type in the Italian industry. Safety Sci 42:587–600.
Fenn P, Ashby S [2004]. Workplace risk, establishment size and union density. Br J Ind Relations 42:461–480.
Fernandes-Alcantara AL [2012]. Youth and the labor force: background and trends. Washington, DC: Congressional Research Service.
Flynn MA [2010]. Undocumented status and the occupational lifeworlds of Latino immigrants in a time of political backlash: the workers’ perspective. Master’s Thesis, University of Cincinnati, Cincinnati, Ohio.
Flynn MA [2014]. Safety and today’s diverse workforce: Lessons from NIOSH’s work with Latino immigrants. Professional Safety 59(6): 52-57.
Flynn MA, Check P, Eggerth DE, Tonda J [2013]. Improving occupational safety and health among Mexican immigrant workers: a binational collaboration. Public Health Rep 128(Suppl 3):33–38.
Flynn MA, Sampson JM [2012]. Trench safety: using a qualitative approach to understand barriers and develop strategies to improve trench practices. Intl J Constr Educ Res 8:63–79.
Forst L, Ahonen E, Zanoni J, Holloway-Beth A, Oschner M, Kimmel L, Martino C, Rodriguez E, Kader A, Ringholm E, Sokas R [2013]. More than training: community based participatory research to reduce injuries among Hispanic construction workers. Am J Ind Med 56(8):827–837.
Gany F, Dobslaw R, Ramirez J, Tonda J, Lobach I, Leng J [2011]. Mexican urban occupational health in the U.S.: a population at risk. J Commun Health 36(2):175–179.
Gillen M, Kools S, McCall C, Sum J, Moulden K [2004]. Construction managers’ perceptions of construction safety practices in small and large firms: a qualitative investigation. Work 23:233–243.
Gomberg-Muñoz R [2010]. Willingness to work: agency and vulnerability in anundocumented immigrant network. Am Anthropol 112(2):295–307.
Grzywacz JG, Quandt SA, Marín A, Summers P, Lang W, Mills T, Evia C, Rushing J, Donadio K, Arcury TA [2012]. Occupational injury and work organization among immigrant Latino residential construction workers. Am J Ind Med 55(8):698–706.
Hasle P, Kvorning LV, Rasmussen CD, Smith LH, Flyvholm MA [2012]. A model for design of tailored working environment intervention programmes for small enterprises. Safety Health Work 3:181–191.
Hasle P, Limborg HJ [2006]. A review of the literature on preventive occupational health and safety activities in small enterprises. Industr Health 44:6–12.
Hecker S, Goldenhar LM [2014]. Understanding safety culture and safety climate in construction:existing evidence and a path forward, http://www.cpwr.com/sites/default/files/publications/hecker_goldenhar_lit_review_ summary_final_0.pdf.
Headd B [2010]. An analysis of small business and jobs. Washington, DC: U.S. Small Business Administration.
Holizki T, Nelson L, McDonald R [2006]. Injury rate as an indicator of business success. Industr Health 44:166–168.
Holte KA, Kjestveit K, Lipscomb HJ [2014]. Company size and differences in injury prevalence among apprentices in building and construction in Norway. Safety Sci 71(C):205–212.
Hope JB, Mackin PC [2007]. The relationship between employee turnover and employee compensation in small business. Washington, DC: Office of Advocacy, U.S. Small Business Administration, http://www.sba.gov/advo/research/rs308tot.pdf.
Huang YH, Ho M, Smith GS, Chen PY [2006]. Safety climate and self-reported injury: assessing the mediating role of employee safety control. Accid Analysis Prev 38:425–433.
Hung YH, Winchester WW 3rd, Smith-Jackson TL, Kleiner BM, Babski-Reeves KL, Mills TH 3rd [2013]. Identifying fall-protection training needs for residential roofing subcontractors. Appl Ergo 44(3):372–380.
Jeong BY [1998]. Occupational deaths and injuries in the construction industry. Appl Ergo 29:335–360.
Knight EB, Castillo DN, Layne LA [1995]. A detailed analysis of work-related injury among youth treated in emergency departments. Am J Ind Med 27:793–805.
Kochhar R [2014]. Latino jobs growth driven by U.S. born: immigrants no longer the majority of Hispanic workers. Hispanic Trends Project, June. Washington, DC: Pew Research Center.
Kotey B, Folker C [2007]. Employee training in SMEs: effect of size and firm type—family and nonfamily. J Small Bus Mgmt 45:214–38.
Krieger N [2010]. Workers are people too: societal aspects of occupational healthdisparities—an ecosocial perspective. Am J Ind Med 53(2):104–115.
Krieger N, Waterman PD, Hartman C, Bates LM, Stoddard AM, Quinn MM, Sorensen G, Barbeau EM [2006]. Social hazards on the job: workplace abuse, sexual harassment, and racial discrimination. A study of black, Latino, and white low-income women and men workers in the United States. Intl J Health Serv 36(1):51–85.
Labor and Occupational Health Program (LOHP) [2015]. Small business resources, http://lohp.org/small-business-resources/.
Landsbergis PA, Grzywacz JG, LaMontagne AD [2014]. Work organization, job insecurity, and occupational health disparities. Am J Ind Med 57(5):495–515.
Mardis AL, Pratt SG [2003]. Nonfatal injuries to young workers in the retail trades and services industries in 1998. J Occup Environ Med 45:316–323.
Mendeloff J, Nelson C, Ko K, Haviland A [2006]. Small business and workplace fatality risk: an exploratory analysis. Technical Report TR-371-ICJ. Santa Monica, CA: RAND.
Miller TR, Waehrer GM [1998]. Costs of occupational injuries to teenagers, United States. Injury Prev 4(3):211–217.
Morisi TL [2008]. Youth enrollment and employment during the school year. Monthly Labor Rev 131:51–63.
Morse T, Dillon C, Weber J, Warren N, Bruneau H, Fu R [2004]. Prevalence and reporting of occupational illness by company size: population trends and regulatory implications. Am J Ind Med 45:361–370.
Mortimer J [2013]. Work and its positive and negative effects on youth’s psychosocial development. In: Runyan CW, et al., eds. Health and safety of young workers: proceedings of a U.S. and Canadian series of symposia. Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; and Ontario Neurotrauma Foundation.
Nicholson VT, Bunn TL, Costich JF [2008]. Disparities in work-related injuries associated with worker compensation coverage status. Am J Ind Med 51:393–398.
NIOSH [2003]. Preventing deaths, injuries, and illnesses of young workers, http://www.cdc.gov/niosh/docs/2003-128/pdfs/2003128.pdf.
NIOSH [2004a]. Sixteen-year-old Hispanic youth dies after falling from a job-made elevated work platform during construction: South Carolina, http://www.cdc.gov/niosh/face/In-house/full200406.html.
NIOSH [2004b]. Two Hispanic construction laborers (ages fifteen and sixteen) die after trench collapse: South Carolina, http://www.cdc.gov/niosh/face/In-house/full200307.html.
NIOSH [2008]. Hispanic construction worker dies while operating ride-on roller/compactor: South Carolina, http://www.cdc.gov/niosh/face/In-house/full200706.html.
NIOSH [2014]. Youth@Work: Talking Safety curriculum. DHHS (NIOSH) Publication Number 2014-109, http://www.cdc.gov/niosh/talkingsafety/states/ri/2014-109/default.html.
NIOSH [2015]. Young worker safety and health, http://www.cdc.gov/niosh/topics/youth/.
Nissen B, Angee A, Weinstein M [2008]. Immigrant construction workers and health and safety: the south Florida experience. Labor Studies J 33(1):48–62.
NRC [1998]. Youth at work: health, safety, and development of working children and adolescents in the United States. Washington, DC: National Academy Press.
O’Connor T, Flynn MA, Weinstock D, Zanoni J [2014]. Occupational safety and health education and training for underserved populations. New Solutions 24(1):83–106.
O’Connor T, Loomis D, Runyan C, Abboud dal Santo J, Schulman M [2005]. Adequacy of health and safety training among young Latino construction workers. J Occup Environ Med 47(3):272–277.
Okechukwu CA, Souza K, Davis KD, de Castro AB [2014]. Discrimination, harassment, abuse, and bullying in the workplace: contribution of workplace injustice to occupational health disparities. Am J Ind Med 57(5):573–586.
Olsen K, Legg S, Hasle P [2012]. How to use programme theory to evaluate the effectiveness of schemes designed to improve the work environment in small businesses. Work 41:5999–6006.
OSHA [2014]. Updates to OSHA’s recordkeeping rule: who is required to keep records and who is exempt. OSHA Fact Sheet, https://www.osha.gov/recordkeeping2014/OSHA3746.pdf.
Page K [2009]. Blood on the coal: the effect of organizational size and differentiation on coal mine accidents. J Safety Res 40:85–95.
Passel JS, Cohn D, Lopez MH [2011]. Census 2010: 50 million Latino Hispanics account for more than half of nation’s growth in past decade. Washington, DC: Pew Research Center.
Pedersen DH, Sieber WK [1988]. National Occupational Exposure Survey, volume 3: analysis of management, interview responses. Cincinnati, OH: U.S. Department ofHealth and Human Services, Public Health Service, Centers for Disease Control, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 89–103.
Pedersen BH, Hannerz H, Christensen U [2012]. The effect of enterprise size on the risk of hospital treated injuries among all male manual construction workers in Denmark, 2000–2006. Safety Sci Monitor 15(4):1–11.
Peek-Asa C, Erickson R, Kraus JF [1999]. Traumatic occupational fatalities in retail industry, United States 1992–1996. Am J Ind Med 35:186–191.
Pew Hispanic Center [2008]. U.S. population projections: 2005–2050. Washington, DC: Pew Research Center.
Polivka AE [1996]. A profile of contingent workers. Monthly Labor Rev 119:10–21.
Rauscher KJ, Myers DJ [2008]. Socioeconomic disparities in the prevalence of work-related injuries among adolescents in the United States. J Adolesc Health 42(1):50–57.
Rauscher KJ, Myers D, Runyan CW, Schulman M [2012]. Young worker safety in construction: do family ties and workgroup size affect hazard exposures and safety practices? Work J Prev Assess Rehab 42:549–558.
Richardson S, Windau J [2003]. Fatal and nonfatal assaults in the workplace, 1996 to 2000. Clin Occup Environ Med 3;673–689.
Runyan CW, dal Santo J, Schulman M, Lipscomb HJ, Harris TA [2006]. Work hazards and workplace safety violations experienced by adolescent construction workers. Arch Pediatr Adolesc Med 160(7):721–727.
Runyan CW, Zakocs RC [2000]. Epidemiology and prevention of injuries among adolescent workers in the United States. Ann Rev Public Health 21(1):247–269.
Schenker MB [2010]. A global perspective on migration and occupational health. Am J Ind Med 53:329–337.
Scruggs K, Arroyo MG [2014]. Latino construction worker resources collection. Silver Spring, MD: CPWR: The Center for Construction Research and Training.
Sinclair R, Cunningham TR, Schulte P [2013]. A model for occupational safety and health intervention in small businesses. Am J Ind Med 56 (12):1442–1451.
Siqueira CE, Gaydos M, Monforton C, Slatin C, Borkowski L, Dooley P, Liebman A, Rosenberg E, Shor G, Keifer M [2014]. Effects of social, economic, and labor policies on occupational health disparities. Am J Ind Med 57(5):557–572.
Smith CK, Silverstein BA, Bonauto DK, Adams D, Fan ZJ [2010]. Temporary workers in Washington state. Am J Ind Med 53:135–145.
Sokas RK, Jorgensen E, Nickels L, Gao W, Gittleman JL [2009]. An intervention effectiveness study of hazard awareness training in the construction building trades. Public Health Rep 124(Suppl 1):160–168.
Souza K, Steege AL, Baron SL [2010]. Surveillance of occupational health disparities: challenges and opportunities. Am J Ind Med 53:84–94.
Spear LP [2000]. The adolescent brain and age-related behavioral manifestations. Neurosci Biobehav Rev 24(4):417–463.
Steege AL, Baron SL, Marsh SM, Menéndez CC, Myers JR [2014]. Examining occupational health and safety disparities using national data: a cause for continuing concern. Am J Ind Med 57:527–538.
Steinberg L [2005]. Cognitive and affective development in adolescence. Trends Cogn Sci 9(2):69–74.
Steinberg L, Amsel E, Smetana JG [2011]. Adolescent risk taking: a social neuroscience perspective. In: Amsel E, Smetana J, eds. Adolescent vulnerabilities and opportunities: developmental and constructivist perspectives. New York: Cambridge University Press.
Stover B, Wickizer TM, Zimmerman F, Futlgon-Kehoe D, Franklin G [2007]. Prognostic factors of long-term disability in a workers’ compensation system. J Occup Environ Med 49:31–40.
Suruda A, Philips P, Lillquist D, Sesek R [2003]. Fatal injuries to teenage construction workers in the US. Am J Ind Med 44(5):510–514.
Sudhinaraset M, Blum R [2010]. The unique developmental considerations of youth-related work injuries. Intl J Occup Environ Health 16(2):195–201.
Tucker S, Turner N [2013]. Waiting for safety: responses by young Canadian workers to unsafe work. J Safety Res 45:103–110.
U.S. Census Bureau [2011]. Statistics for all U.S. firms with paid employees by geographic area, industry, gender, and employment size of firm: 2007, http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=SBO_2007_00CSA09&prodType=table.
US Census Bureau [2014a]. Annual Estimates of the Resident Population by Sex, Age, Race, and Hispanic Origin for the United States and States: April 1, 2010 to July 1, 2013 http://factfinder.census.gov/faces/tableservices/ jsf/pages/productview.xhtml?pid=PEP_2013_PEPASR6H&prodType=table
U.S. Census Bureau [2014b]. 2010–2014 March supplement to the Current Population Survey: calculations by CPWR Data Center. Silver Spring, MD: CPWR—The Center for Construction Research and Training.
U.S. DOL [2013]. Child labor provisions for nonagricultural occupations under the Fair Labor Standards Act, http://www.dol.gov/whd/regs/compliance/childlabor101_text.htm#6.
van der Molen HF, Lehtola MM, Lappalainen J, Hoonakker PLT, Hsiao H, Haslam R, Hale AR, Frings-Dresen MHW, Verbeek JH [2012]. Interventions to prevent injuries in construction workers. Cochrane Database Systematic Rev 12:CD006251.
Walter N, Bourgois P, Loinaz LH, Schillinger D [2002]. Social context of work injury among undocumented day laborers in San Francisco. J Gen Intern Med 17:221–229.
Wojcik SM, Kidd PS, Parshall MB, Struttmann TW [2003]. Performance and evaluation of small construction safety training simulations. Occup Med 53:279–286.
Zakocs RC, Runyan CW, Schulman MD, Dunn KA, Evensen CT [1998]. Improving safety for teens working in the retail trade sector: opportunities and obstacles. Am J Ind Med 34(4):342–350.
Zierold KM, Anderson HA [2006]. Severe injury and the need for improved safety training among working teens. Am J Health Behav 30(5):525–532.
Disclaimer, Ordering Information, Suggested Citation
Disclaimer
Mention of any company or product does not constitute endorsement by the National Institute for Occupational Safety and Health (NIOSH). In addition, citations of websites external to NIOSH do not constitute NIOSH endorsement of the sponsoring organizations or their programs or products. Furthermore, NIOSH is not responsible for the content of these websites. All Web addresses referenced in this document were accessible as of the publication date.
Ordering Information
To receive documents or other information about occupational safety and health topics, contact NIOSH at
Telephone: 1–800–CDC–INFO (1–800–232–4636)
TTY: 1–888–232–6348
E-mail: cdcinfo@cdc.gov
or visit the NIOSH website at www.cdc.gov/niosh.
For a monthly update on news at NIOSH, subscribe to NIOSH eNews by visiting www.cdc.gov/niosh/eNews.
Suggested Citation
NIOSH, ASSE [2015]. Overlapping vulnerabilities: the occupational safety and health of young workers in small construction firms. By Flynn MA, Cunningham TR, Guerin RJ, Keller B, Chapman LJ, Hudson D, Salgado C. Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 2015-178.